Introduction
National Health Plans must include surgery, obstetric, and anaesthesia (SOA) services to achieve Universal Health Coverage.1,2 Recognition of this need has increased, with the Republic of Zambia, Republic of Tanzania, Madagascar, Malawi, Zimbabwe, and Namibia developing national surgical healthcare policies. However, other Southern African Development Community (SADC) Member States lag behind in policy development.3,4
National Surgical, Obstetrics and Anaesthesia Plans (NSOAPs) were proposed by the Lancet Commission on Global Surgery as a policy framework that Ministries of Health could use to evaluate and strengthen their health systems’ capacity to deliver surgical, obstetric and anaesthetic (SOA) care.5 These plans align with Member State political commitments contained in World Health Assembly (WHA) resolution 68.15, which affirmed the importance of safe, timely and affordable access to emergency and essential SOA care as a component of Universal Health Coverage.6 This commitment was recently reaffirmed with the adoption of WHA resolution 76.2.7 SADC Member States led the negotiations for the adoption of WHA68.15 and have committed to developing NSOAPs, sharing best practice through a ‘peer review’ mechanism that includes reporting progress at annual SADC Health Ministers’ meetings and participation within the SADC Technical Experts’ Working Group (SADC-TEWG) on SOA care.
Of the 16 SADC Member States, 38% (n=6) have completed NSOAP development, while 62% (n=10) are at different stages of development of national surgical healthcare policies as reported at the monthly SADC-TEWG Situation Room meeting.8 Other African countries (Rwanda, Ethiopia, and Nigeria) have implemented similar policies.9–11 Globally, the Western Pacific Region has also developed a Regional Action Framework for National Surgical Planning and Development,12 Pakistan has published a National Vision for Surgical Care13 and Ecuador has begun developing an NSOAP – the first in Latin America.14 Despite many national surgical plans being created worldwide, only Ethiopia has performed an audit of the surgical healthcare improvement policy’s implementation process.15
Notwithstanding the COVID-19 pandemic, progress in NSOAP development has been slower than anticipated.16 With the expiry of the 2030 agenda for sustainable development approaching, it is important to elucidate barriers that impede the development and implementation of national surgical healthcare policies. Information delineating enabling or delaying factors could prove critical in the formulation of strategies to support and accelerate surgical health policy formulation in the region, and inform directions that other countries might take.
This is a cross-sectional survey to identify barriers (leadership, political, economic, logistical, administrative, technical or other) to NSOAP policy development and implementation in the 16 SADC Member States. The primary aim is to describe the main barriers to NSOAP development. Secondary aims are to identify (1) facilitators of NSOAP development and (2) barriers to NSOAP implementation.
Methods
Study design and participant inclusion criteria, survey instrument design, survey dissemination and administration plan, analysis plan, and ethics approval are reported as per the Checklist for Reporting Results of Internet E-Surveys (CHERRIES), guidelines for reporting internet based e-surveys.17
Study Design and Participants
This was a cross-sectional survey of stakeholders of surgical care within SADC Member States. Invited stakeholder groups included - but were not limited to - government, hospital management, healthcare professionals, non-governmental organisations, academic institutions, professional associations, World Health Organisation representatives, and donors. There was no financial incentive; participation was purely voluntary.
Participants were recruited using purposive, snowball, and convenience sampling. The initial recruitment phase was limited to recommended contacts within the SADC SOA community through the SADC-TEWG. Respondents suggested expanding access via various SOA-specific WhatsApp group platforms to improve participation. A second recruitment phase with an open survey link was launched, followed by a third phase of purposive follow-up of stakeholders from Member States that were under-represented.
Survey Instrument
We designed a structured questionnaire (Appendix 1) comprising the following sections: demographic information including country representation and stakeholder type; and respondents’ perceptions of 1) government support for NSOAPs; 2) existence of an NSOAP task force; 3) resources for NSOAP development; and 4) NSOAP development as per the domains of the NSOAP manual18: a) situation analysis and baseline assessment; b) stakeholder engagement and priority setting; c) drafting and validation; d) monitoring and evaluation; e) financing; and f) governance. For those respondents from countries in which an NSOAP already existed, there was a section on implementation.
The survey was created in English. Translated versions were available via a Google Chrome plugin for respondents in Angola (Portuguese), DRC, and Comoros (French). Study data were collected, managed, and stored using secure REDCap software.19,20 Adaptive questioning utilising REDCap branching logic function was employed. The tool was piloted by three individuals outside the design team to refine the content, structure, branching logic, general useability and technical functionality before final dissemination. The survey could be completed via computer or smartphone.
Utilisation of the adaptive questioning technique precluded a completeness check. Completion of at least six questions was required for response inclusion; the maximum number of questions was 76. The survey ranged from 2-14 sections (pages).
Survey Dissemination and Administration
Phase 1 occurred from September to October 2022. Known stakeholders within SADC were invited to participate via email. The survey was launched at a SADC-TEWG meeting and promoted via the SADC SOA WhatsApp group by its Chair and the study team.
Phase 2, from November to December 2022, introduced an open recruitment process via WhatsApp to appropriate groups, e.g. the Zambian Surgeons’ professional network, the Namibian NSOAP development group, and the Surgical Society of Botswana network.
During phase 3 (January to February 2023), purposive recruitment of stakeholders from Member States that were underrepresented took place. These individuals were identified and contacted via email and/or WhatsApp.
We expressly permitted participants to complete the survey more than once if responding for multiple member states. The risk for duplicate entries could theoretically not be excluded but there was no behavioural incentive for this.
Analysis
Responses were evaluated for completeness. Due to the adaptive questioning technique, survey length differed between participants. If a participant had not completed the entirety of their bespoke survey, but had completed at least one section beyond demographic information, this was counted as a partial response and included in the analysis as such. Participants were counted as having completed the survey in entirety if they completed all fields up to and not including optional questions following the survey about continuing collaboration within the SADC-TEWG.
We did not use weights to improve representativeness but conducted a post-hoc subgroup analysis of responses from the Republic of Zambia, as these accounted for 38% of the responses. Entries that did not have a minimum demographic data set (SADC Member State and stakeholder group) were excluded from analysis. Data were de-identified prior to analysis. Basic descriptive statistics were conducted using Microsoft Excel for quantitative data. A thematic analysis for major themes was carried out for qualitative responses.
Ethics
IRB exemption was determined by the Institutional Review Board of Harvard Medical School (IRB22-0262), and full ethics approval granted by the Human Research Ethics Committee of Witwatersrand University (HREC: M220250). A participant information sheet was included as the initial page of the survey, requiring affirmative consent before the survey could proceed. Only the research team had access to the REDCap database.
Results
Response and completion rates
In phase 1, individualised survey links were sent to 342 unique email addresses. Of these, 55 logged at least a partial response, equating to a response rate of 16%. This prompted phase 2 and 3 of recruitment.
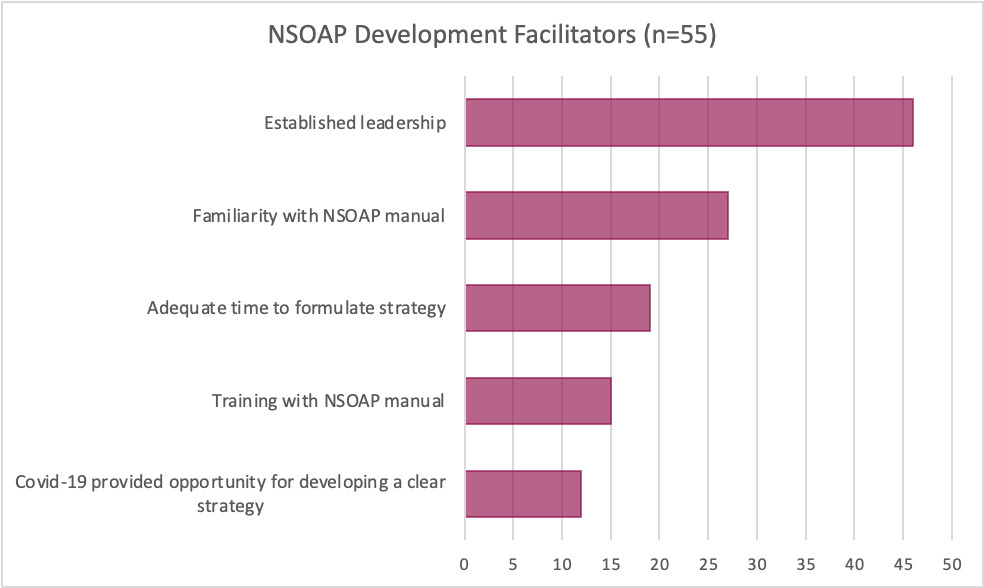
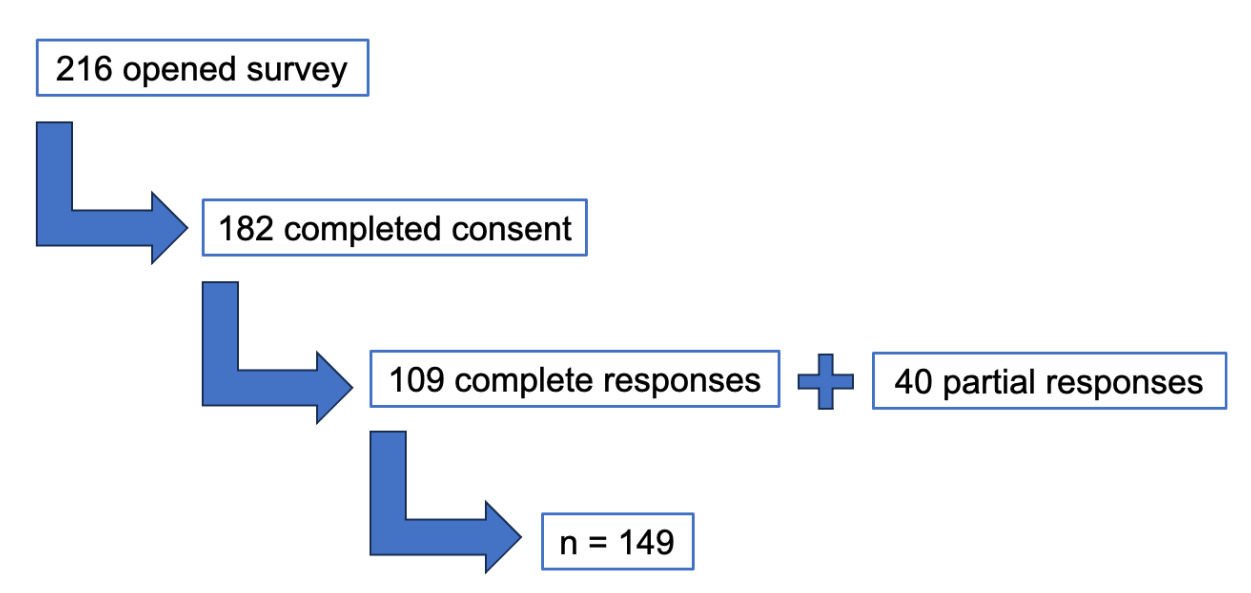
Following all recruitment phases, 216 participants opened the survey and 84% (n=182) completed at least the consent form. Completion rate was 60% (109/182). An additional 40 participants recorded partial responses. Over the three periods of data collection, 149 partial and complete responses were obtained (Figure 1).
Respondent Demographics
Responses were obtained from 87% (n=14) of countries; there were no responses obtained from Mauritius or Mozambique. Figure 2 graphically presents country-level representation. Respondents represented the following stakeholders: 60% health care professionals (n=90), 24% government (n=36) and 23% academic institutions (n=34). Of 149 respondents, 30% (n=45) respondents held memberships in multiple stakeholder groups (median 1; range 2-5) and two responded ‘other’ but did not provide an alternative affiliation (Table 1). 140 participants responded to the question, ‘Are you satisfied with the overall quality of surgical services in your country?’ of which 93% said that they were not. Although respondents were often self-identified members of professional and governmental groups, all responses were analysed as representing the viewpoint of the individual rather than any organisation.
Free text responses to ‘strengths and weaknesses’ questions
The survey requested that respondents express at least one strength and one weakness of surgical services in their country. Responses were categorised thematically into responses regarding infrastructure, SOA staffing, and outcomes. In terms of strengths, respondents were optimistic about the breadth and availability of procedures: 25% (n=31/124) respondents commented on availability of surgical procedures and operating theatre space, increasingly at district (level 1) or regional/provincial (level 2) hospitals. Further, 11% (n=14) respondents commented on the existence of a referral system and access to tertiary level care. Twenty-seven percent (n=34) of respondents indicated adequate numbers of staff exist, and that the number of specialists, specialist training, and basic surgical training for non-specialist doctors was increasing. Ten percent (n=12) of respondents commented on the commitment and passion of specialists to provide SOA care. Another strength was the reported low- or no-cost surgical services for impoverished patients through government-led health programmes, which was mentioned in 7% (n=9) of responses.
Challenges regarding infrastructure, equipment and medical-surgical supply challenges were the most reported weakness. Twenty-eight percent (n=40/143) respondents cited inadequate, obsolete diagnostic and surgical equipment and 17% (n=24) reported a lack of consumables and medications as weaknesses of their surgical systems. In addition, 17% (n=24) commented on the persistent low number of specialist doctors and specialised ancillary staff, including nurses and scrub technicians. Respondents also flagged challenges with inequitable distribution of surgical services between urban and rural regions, between rural regions, and an overall lack of policy or guidelines regarding quality and provision of care. Despite the increasing scope of procedures offered, respondents indicated that tertiary centres were overwhelmed and there were long wait-times for emergency and elective procedures. One respondent wrote of ‘significant waiting times both for elective as well as emergency surgeries. Many patients do not have adequate access to surgical services and the delay contributes to morbidity and mortality’. Interestingly, three respondents reported that reliance on private health systems resulted in lack of investment in public systems and thus poor quality of care for the uninsured population. One respondent stated: ‘There is [a] HUGE gap between state (government) and private health care. Almost 88% patients use state facilities and only 12% private facilities. The resource allocation is less than 12% for government patients’.
Political Landscape, Task Force Development, and Resources
When asked about perceptions of the political will surrounding NSOAP development and implementation, 47% (n=56/119) stated that their government supported NSOAP development ‘a little’. Twenty-seven percent (n=32) reported that their government ‘supports and is driving’ the NSOAP development process.
There were 135 responses with 30% (n=41) responding ‘unknown’ to whether a task force for NSOAP development existed in their country. Of the other responses, 28% (n=35) believed that the NSOAP Development Task Force was unaffected by the COVID-19 pandemic, and 21% (n=28) believed that key members of the task force were redirected to COVID-19 efforts. Twenty-one percent of respondents (n=28) reported no task force existed in their respective countries. Reasons cited were ‘no champion to lead the NSOAP process’, ‘not enough interested people to create a task force’, '‘stakeholders have competing interests preventing the formation of a cohesive working group’ and ‘lack of focus’. Where there was a task force, 61% (n=40) reported coordination between members.
Stakeholders were asked to select which entities they believed provided financial and/or personnel resources for NSOAP development (Figure 3). Eight different potential sources of resources were offered (as well as the options of ‘none’ and ‘other’). Forty-three percent of respondents (n=64) reported provision of personnel resources; within this group, the median number of selected sources was 3 (range 1-8) and total number of selections was 190. Personnel assistance included support for data collection, policy drafting, advocacy efforts, and similar tasks. Personnel resources were perceived to be sourced from national governments (24%, n=45), domestic universities (20%, n=38), foreign universities (14%, n=27), and the SADC-TEWG (11%, n=21). Thirty-five percent of respondents (n=52) reported financial provision. Within this group, the median number of selected sources was 2 (range 1-5) and the total number of selections was 103. National government constituted 25% (n=26) of selections; WHO constituted 23% (n=24), and international organisations like the World Bank constituted 16% (n=16).
Free text responses to factors that affected political support of NSOAP development
Free text answers were elicited in response to the question ‘Please specify any other factors that may have influenced political support of NSOAP development, and whether this has resulted in an increase or decrease in support of NSOAP development’. Respondents listed factors that they believed both increased and decreased political support fairly equally. With regards to decreasing support, the most commonly cited reasons were high turnover of key personnel in government positions and other health priorities (including COVID-19) taking precedence over SOA care. Other factors cited were decreasing donor support, other political priorities (e.g. eastern DRC conflict), and lack of awareness of SOA care needs. Regarding factors that increased political support for NSOAP development, the most commonly reported was the dedication of leadership and advocacy teams and personnel in putting pressure on the government. One respondent wrote, ‘The resilience of the technical team in advocating for NSOAP development and implementation has influenced the political leadership to pay more attention’. Others cited external pressure from NGOs to increase access to SOA care, as well as restructuring of governmental agencies and human resources providing increased capacity toward NSOAP development.
NSOAP Development Barriers
Respondents were asked whether an NSOAP process had been initiated in their country; of 73 respondents, 68% (n=50) said the process had been initiated, 8% (n=6) that it had not been initiated, and 23% (n=17) were unsure. The 50 respondents who were aware of an NSOAP process being initiated in their countries were asked to indicate which of the following domains presented challenges in NSOAP development: situational analysis and baseline assessment; stakeholder engagement and priority setting; drafting and validation; monitoring and evaluation; finance; governance; or none. Figure 4 provides a detailed account of all responses and the specific components of each domain that presented a challenge in the NSOAP development process. Financing, stakeholder engagement and priority setting, and situational analysis and baseline assessment were the three categories that were most often cited as having presented challenges to NSOAP development.
NSOAP Implementation
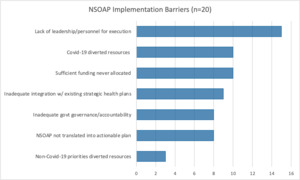
Three countries had begun NSOAP implementation at the time of survey distribution: Zambia, Tanzania, and Madagascar. Participant stakeholders from these countries were asked about barriers to implementation in addition to barriers to development. Of these, there were 34 responses regarding Ministry of Health support for implementation: 59% (n=20) reported that the Ministry of Health supported implementation ‘a little’, and 26% (n= 9) reported that the Ministry of Health ‘supports and is driving the NSOAP implementation process.’ In response to the question ‘Has implementation gone to plan?’ zero respondents said ‘yes’, 21% (n=6) of 28 said ‘no’, and 50% (n=14) said ‘partially’. The six respondents who responded ‘no’ and 12/14 ‘partially’ responses were submitted by Zambian respondents, as well as the majority of responses regarding implementation barriers (90%, n=18/20). Of eight potential barriers, respondents indicated that seven were applicable (with 7-10 responses for each) in their context. Mirroring the stated barriers for NSOAP development, there were issues around finance and personnel resources as well as inadequate leadership and governance. However, there were additional implementation barriers around the NSOAP not being translated into an actionable plan, and inadequate integration of the NSOAP into the National Health Strategic Plans (NHSP). Notably, unlike the responses to the questions about barriers to NSOAP development, respondents from all 3 countries (Zambia, Madagascar, and Tanzania) said that COVID-19 did, in fact, divert resources from NSOAP implementation (Figure 5).
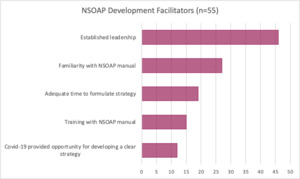
NSOAP Development Facilitators and Positive Effects of NSOAP Implementation
Regarding factors that facilitated formulation of an NSOAP development strategy, of 119 responses, 39% (n=46) reported the presence of established leadership as a driving factor (Figure 6). Regarding positive effects of NSOAP implementation, or positive changes in the status of SOA care in their country since implementation was due to start, 18% reported benefits in improved access to emergency surgical care (n=13/72), 21% reported improved provider workforce with regards to SAO specialists (n=15) and 13% with regard to non-specialists including nurses (n=9). Eleven percent (n=8) reported that there has not been any positive change in surgical care since their NSOAP was published.
Negative aspects of NSOAP Development or Negative Changes in Surgical Health Care
Respondents were asked about the negative effects of NSOAP development and implementation, as well as other negative changes to surgical systems they have perceived since the time NSOAP implementation began. There were no responses from Madagascar and Tanzania; a few free-text responses were given by Zambian respondents. These responses included concerns about lack of specialist training, decreased number of specialists compared to increasing workload, lack of funding for operations and need for patients to purchase their own surgical supplies, and depleted surgical support services leading to increased case cancellations. On a structural level, one respondent reported a lack of engagement and advocacy for surgical healthcare at the community level.
Zambia Subgroup Analysis
Since 38% (n=56) of the 149 total responses were reported for Zambia, these responses were analysed separately as a subgroup as well as within the complete response analyses reported above. Responses in all categories closely mirrored the responses received for the entire cohort. A comparison of the responses from the Zambian subgroup and the total dataset are reported in Figure 7.
Regarding resources, respondents perceived higher provision of personnel resources (n=48) than financial resources (n=30). Likewise, personnel resources were perceived as being supplied by the national government (31%, n=15) and universities (33%, n=16), whereas financial resources were perceived to be supplied by WHO (17%, n=5), foreign governments (23%, n=7), or other international organisations e.g. the World Bank (23%, n=7). Two other sources of personnel resources mentioned were surgical societies and the Zambia Medical Association.
Regarding implementation of Zambia’s NSOAP, 12 of the respondents reported being involved with the implementation process and 23 reported that they were not involved.
Discussion
Government decision agendas depend on the alignment of problem, policy, and political streams.21 Concerning surgical healthcare, the problem remains as urgent as ever, so an opening of a policy window relies on having enough governmental political will to drive successful policy reform. The gains are potentially far-reaching: the top-down directive to strengthen a surgical system would ultimately strengthen the entire national health system.22 However, our survey results indicate the perception of limited political conviction for national surgical healthcare policy in many SADC Member States. Taken at face value, it raises the question of why there is so little impetus to strengthen SOA care. This study was not designed to explore that specific issue, but Mhazo et al have specifically looked into the ‘lack of political will’ for health reform in sub-Saharan Africa, elucidating more specific drivers: ‘1) the distribution of costs and benefits arising from policy reforms, 2) the form and expression of power among actors, 3) the desire to win or stay in government, 4) political ideologies, 5) elite interests and 6) policy diffusion’.23 Other potential factors include a lack of state capacity24 in LMIC governments and potentially a lack of lobbying power.25 However, this study indicates that where there is an existing strategy to incorporate adequate minimal standards for surgical care within the national health plan, the key driver has been perceived as established leadership of the process within the Ministry of Health.
In terms of the technical process of NSOAP formulation, finance was the most commonly cited component that presented difficulty. This was principally thought to be due to the absence of an allocated budget for surgical system strengthening within the Ministry of Health and a lack of accurate costing data. Notably, there were relatively few respondents who thought that a lack of economics or financial expertise was the main cause. Most respondents reported being unaware how the NSOAP process was being resourced. It is no surprise that finance was perceived as the greatest challenge; LMICs are, by definition, resource-limited; and much of sub-Saharan Africa continues to be reliant on external aid to finance healthcare services.26,27 Furthermore, formulating a policy without the certainty of funding for implementation might be perceived by the electorate as an empty or broken promise and compromise the prospect of re-election for the sitting government.
Stakeholder engagement was the second most commonly cited challenge. Within this theme, there have been difficulties engaging with key stakeholders from both public and private sectors, and agreeing who these key stakeholders are. Another highlighted difficulty is competing interests between key stakeholders. Given the diversity of stakeholders, it goes without question that different goals exist for SOA care delivery and development. Within this diverse cohort, there must be intentionality in the choices made regarding which voices to include and which to prioritise. This can only happen if clear government leadership of the process is established.
Voluntary participation inevitably gives rise to self-selection bias; 60% of respondents were healthcare providers, 24% represented government and 23% from academic institutions (with overlap of these cohorts), but there was minimal representation from intergovernmental organisations (such as the World Bank and World Health Organisation) and no representation from donor agencies or private industry. This could relate to dissemination techniques, and/or the level of engagement from these stakeholders with regard to NSOAP development. The authors re-evaluated the initial closed survey methodology in light of the low response rate (16%) and general feedback from participants but ultimately, responses were limited to what networks could be accessed. Frontline healthcare providers would be unlikely to access networks of the private sector, potential donors, government treasury and intergovernmental organisations, to whom the authors also lacked direct access.
The lack of engagement with these sectors is in itself a barrier. As previously highlighted, innovative plans to incorporate surgical care into national health care cannot be formulated and implemented without appropriate funding, making potential funders (both domestic and international) some of the most influential stakeholders. However, they are notably absent from the discussion. Furthermore, there was no representation of civil society among the respondents. To our knowledge, patient representative groups have not been formally consulted for any of the six previously-published national surgical plans in the SADC region.
Self-selection bias and dissemination via the WhatsApp platform also resulted in uneven representation from different countries within SADC, with Zambia providing 38% of the total responses whilst none were elicited from Mozambique or Mauritius. The diversity between SADC Member States should not be underestimated, and thus skewed representation is a significant limitation. The post-hoc subanalysis of Zambian responses was performed to address this, which largely reflected the findings of the overall cohort. There was one notable difference in that financing was the third most cited barrier to development rather than the first. This finding could be due to the leadership and engagement of the Zambian Ministry of Health in the NSOAP development process, and local funding was made available for policy development, overcoming immediate financial barriers.
The implication of this study is that advocating for national surgical healthcare policy to be formulated is not sufficient to achieve policy development, much less implementation and achieving measurable impact on population health. The financial barrier is the most significant, and there are lessons to learn from the wider Global Health community in this regard. Firstly, the priority should be to increase domestic government health financing for obvious sustainability reasons28; but secondly, donor agencies (such as PEPFAR and the Global Fund) have been transformative in recent decades.29,30 The surgical community has much to learn from the positive impact of such funds, as well as the unintended negative consequences on health systems31 which should be mitigated against. It follows that the next step is to engage decision makers and funders (national treasury, intergovernmental and non-governmental organisations, philanthropies, private industry, etc.) from the very beginning, and align their interests to envision a sustainable financing model for surgical healthcare.
The NSOAP Manual,18 in its static form, is intended to be a template to guide LMICs through the technical process of creating a policy to address lack of access to emergency and essential surgical, obstetric, and anaesthesia care, including trauma, critical and perioperative nursing care. Whilst many countries have embarked upon this process, lack of robust monitoring and evaluation processes with standardised metrics has made it difficult to gauge what impact this has made on surgical healthcare provision. The end goal of any intervention in the global surgery space is to increase access to and quality of surgical healthcare. Policy formulation is a vehicle to support that aim, rather than an end in itself. In order to ensure that national surgical planning process achieves the goals of improved surgical healthcare for all, it is critical to incorporate ongoing evaluation of the policy against its stated goals as part of its development process.
Conclusions
Among LMICs, development of national strategies and specific plans to implement appropriate levels of surgical healthcare has been slow. In seeking to delineate barriers (and appreciating inter-country variability), financing and political will have emerged as the most commonly cited challenges within SADC. Decision makers and potential funders should be engaged early, to envision a sustainable financing model for surgical healthcare.
.png)



.png)