1. INTRODUCTION
Abdominal wound dehiscence (AWD) is a mechanical failure of a healing abdominal surgical wound. The incidence of abdominal wound dehiscence ranges from 0.4 to 3.5%, and it can reach 10% in the elderly. The associated mortality rate reaches up to 45%.1–9 Several studies identify various combinations of factors as risk factors, which are typically classified as local and Systemic factors.2,10 Patient-related comorbidities and procedure-related parameters such as surgery type, incision and closure type, and operation time are among the risk factors. Nevertheless, wound infection is the most crucial factor.7,9,11–15
AWD remains a serious postoperative complication despite technological and surgical advancements. This is predominantly due to the influence of patient-specific factors.8,16,17 AWD is regarded as a reliable indicator of patient safety due to its influence on morbidity, duration of hospital stay, including intensive care therapy, readmission rate for another surgery, and health care costs.6,8,11,12 AWD and other wound complications increase healthcare costs and prolong hospital stays due to increased morbidity, resulting in significant economic and psychosocial strain on the patient and the healthcare system. The burden AWD places on an already overburdened healthcare system in places like Ethiopia should not be underestimated.14,18–20 There are various modifiable risk factors for AWD that can help reduce the occurrence of this devastating condition. Identifying high-risk patients in advance would enable the surgeon to take preventative measures during surgery, such as the application of a retention suture or the use of absorbable or non-absorbable meshes.6,17
The purpose of this study is to determine the risk factors and magnitude of AWD in two selected hospitals in the Sidama region of Ethiopia. So far, there have been only two reports of this dreadful condition in Ethiopia. The first was performed at St. Paul’s Hospital in Addis Ababa, Ethiopia. The other was done at Tikur Anbessa Specialized Hospital and involved only pediatric patients.2,18 Both studies revealed the magnitude of AWD in their respective contexts, as well as potential risk factors for AWD, including emergency surgery, surgical site infection, and intrabdominal sepsis. Both studies lacked a comparison group to reach their conclusion, which we deemed a major drawback, and the later study only included pediatric cases. Unlike the two studies, this one is a case-control study that includes people of all ages.
2. MATERIALS AND METHODS
2.1. Study site and period
The research was carried out at the departments of surgery at two facilities in the Sidama Region, Hawassa University Comprehensive Specialized Hospital (HUCSH) and Yirgalam hospital medical college, from February to May 2023. The Sidama area is located in southern Ethiopia. The region’s major crops are ‘enset’, wheat, teff, and barley, as well as cereals and coffee as cash crops. Hawassa is the capital city of the Sidama region. It is located 274 kilometers south of Addis Ababa, Ethiopia’s capital city. HUCSH is a tertiary hospital in Hawassa, Ethiopia. It is the only teaching-specialized referral hospital in the region. It is a referral center for patients from the region and nearby areas. It delivers services to almost 20 million people. Yirgalem hospital medical college is 315 kilometers from Addis Ababa. It serves a population of approximately 4 million people.
2.2. Study design
A case-control study was used to find out the risk factors for abdominal wound dehiscence and its frequency in patients who had undergone laparatomy for different reasons at Hawassa University Comprehensive Specialized Hospital (HUCSH) and Yirgalem hospital medical college in the department of surgery.
2.3. Source and study population
The source population was all patients who had undergone laparotomy at the two study hospitals. The study population comprised surgical patients from the surgical departments of the chosen hospitals who underwent laparotomy within the last five years and developed AWD for cases, and controls who underwent laparotomy within the same time frame (April 1, 2018 to January 31, 2023) but did not develop AWD. All pediatric and adult patients who had laparotomies during the five-year period (April1, 2018 to January 31, 2023), both elective and emergency surgeries, were included and patients transferred out, died or referred were excluded
2.4. Data collection and Data analysis
The data were collected using software called the Kobo Toolbox. This was done once a patient was identified from the operation room (OR) log books using a patient-specific identification number (chart number), which was used to retrieve the patient’s chart. Three surgical residents entered the data into the Kobo toolbox. The number of laparotomies was obtained from the OR log books. The operating theater (OR) log book of the selected hospitals was used to identify patients, and data were extracted from April 2018– January 2023. For each identified case of AWD, two controls were selected. Controls were not matched to cases based on any specific characterstics. Controls were people who underwent lararotomy and did not develop AWD. Any two consecutive cases on the OR log book close to the identified case of AWD were taken as controls.
Chart review: Three surgical residents reviewed the patients’ charts. Two residents of HUCSH and one resident of Yirgalem hospital medical college were assigned. Chart numbers were traced from the OR log book, and charts of a specific patient, both a case of AWD and respective controls, were reviewed thoroughly. The data was then entered into the Kobo toolbox. The data included socioeconomic characteristics, preoperative risk assessment, and intraoperative and postoperative risk assessment.
After editing, the data were exported from the Kobo toolbox to SPSS software version 26 for analysis. Descriptive statistics (frequencies and percentages) were used to summarise the study participants relationship to the study variables. Texts, tables, and charts were used to display the results. Chi-squared test ,Fisher’s exact tests, and Mann-Whitney U test were used as appropriate, to explore the association between categorical variables. Univariate binary logistic regression analysis was employed to assess the relationship between individual potential risk factors and the event. Consequently, the factors that were statistically significant (p < 0.05) or clinically pertinent to the event were incorporated into a multivariable binary logistic regression model to ascertain independent predictors. Results were presented using crude odds ratios (COR), adjusted odds ratios (AOR), 95% confidence intervals (CIs), and P-values. All significance tests were two-tailed and P<0.05 was considered significant. Variables which do not fulfill the assumptions of biniary logistic regression were exluded from both univariate and multivariable binary logistic regression analyses.
3.2. Ethical considerations
Ethical clearance was obtained from the Hawassa University College of Medicine and Health Science Institutional Review Board (IRB) and the IRB number is IRB/069/14.
4. RESULTS
We included 196 patients and 63 were cases of abdominal wound dehiscence and 133 were controls. The total number of laparotomies performed during the study period was 3792, of which 1270 (33.5%) were elective and 2522 (66.5%) were emergency procedures. 1206 (31.8%) were pediatric patients, and 2586 (68.2%) were adults. The magnitude of abdominal wound dehiscence in our study was 63 (1.66%).
Socio-demographic characteristics
Out of the study subjects, only five (7.93%) of the cases were above the age of 61. As to place of residence, those from rural areas accounted for 66 (33.67%), while those from urban areas accounted for 48 (24.5%). (Table 1).
Pre-operative conditions
In our study, regarding the preoperative risk assessment, 37 (65%) of cases versus 20 (35%) of controls had anemia, with a P-value of <0.001. The majority of cases underwent (58 of 63, 92.1%) emergency surgery, compared to 86 out of 133 controls (64.7%). (Table 2)
Intraoperative and postoperative risk assessment variables
Regarding the type of surgical incisions, 47 (74.6%) of the cases and 61 (45.8%) of the controls underwent a midline vertical incision, which is the commonest type of incision. Of the hospital deaths, most were cases (13, 76.5%). (Table 3).
In our study, 54 (85.7%) of the cases had an acute abdomen of different etiologies. Intestinal obstruction of various benign pathologies, followed by appendicitis and its complications, were the commonest intraoperative diagnoses among cases of AWD (25 and 15 cases, respectively). (Fig.1)
Abdominal wound dehiscence and its features
58 out 63, 92.1% of the cases developed a complete wound dehiscence. About two-thirds of the cases (42 out of 63, 66.7%) developed WD within 6–10 days after laparotomy. The majority (88.8%) of the cases were re-operated . Exluding those who died, the median length of hospital stay was significantly longer for cases (22 days; IQR: 13.75–30) compared to controls (6 days; IQR: 3–9; p < 0.001, Mann-Whitney U test).(Table 3)
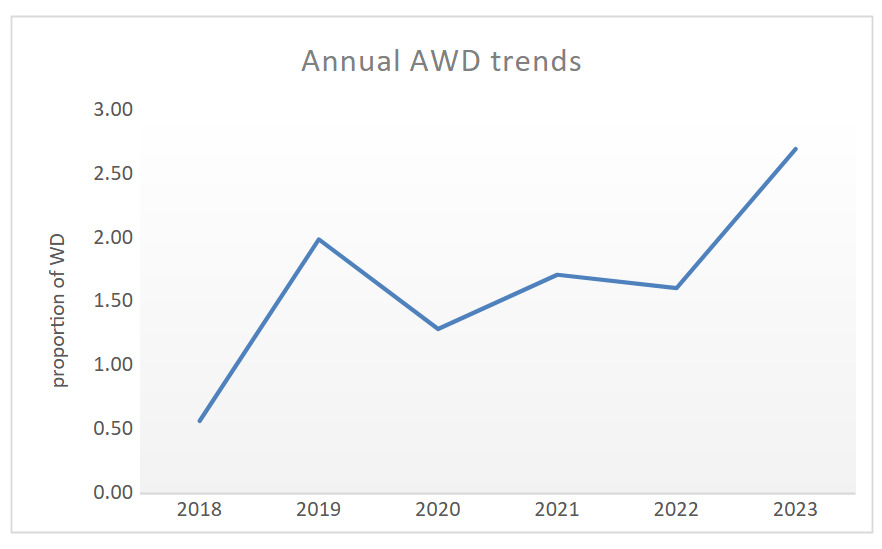
Trend of abdominal wound dehiscence
The trends of AWD in the study hospitals showed decreasing trends from late 2018 to early 2019, and the trend plateaued in the subsequent three years (until late 2021) with a yearly case of 13. However, the trend dropped faster, from 13 to 8 cases in 2022 until early 2023. (Figure 2).
Factors associated with WD
Variables were put into the binary logistic regression model for univariate and multivariable analyses. When possible confounding factors were taken into account, place of residence, anemia, emergency surgery, and the presence of post-operative complications were significantly associated statistically with abdominal wound dehiscence. (Table 4)
5. Discussion
The study found a magnitude of 1.66% and a variety of factors to be statistically linked with AWD in the study area. These included the patients’ residency, post-operative complications (SSI, anastomotic leak, HAP), anemia, and emergency surgery.
This hospital-based study showed that the magnitude of AWD was 63 (1.66%). This was slightly higher than the study done in St. Paul,Ethiopia (0.99%).2 This value is comparable with a study done in Sarajevo and India.6,12,15,16 Even though the incidence differs across hospitals and settings, it is consistent with the global report stating the wound dehiscence (WD) ranges from 0.4–3.5.1–5,7–9 However, in a study done in pakistan, it was 4.42%,3 it was 6.9% in a study done in Argentina10 and a study done in a university set up in Egypt ,the frequency was 7.3%.17 Another study done in addiss ababa,Ethiopia which was on pediatric cases showed an incidence of 7.9%.18 The high incidence in these studies could be due to the presence of multiple comorbidities, poor nurtritional status, delayed presentation, a higher proportion of emergency surgeries or due to advanced age with malignancy or complexity of the surgeries. The other explanation is due to the methodology employed like in21 where it is 12.4% because development of wound dehiscence was studied only in patient population who underwent emergency surgery.
Regarding place of residence, patients who lived in rural areas were statistically more likely to experience AWD than those who didn’t. This discovery has never been mentioned in prior studies. This is one of the study’s original findings. The patients’ poor nutritional status or their delayed presentation to medical facilities due to access or knowledge issues could be the causes, but this variable needs more research.
The study identified postoperative complications as a strong risk factor for AWD and were associated with a twenty-fold increased risk of wound dehiscence. Previous, comparable studies supported our evidence .2,4,5,7,11,15,17,18,20,21
Emergency abdominal surgery was another significant risk factor that was determined to be strongly associated with AWD. Patients who underwent emergency abdominal surgery in this hospital-based study had higher odds of developing AWD (AOR = 10.17) than those who underwent elective procedures. In a case-control study carried out in Poland, this was thoroughly validated.5 The patient’s poor overall health, the high likelihood that the surgical wound will become contaminated, and the possibilities that the surgical team’s performance may be jeopardized are some of the contributing factors. Of the cases in our study, 54 (85.7%) had acute abdomens of various etiologies. This is consistent with a number of other studies, including those conducted in Egypt and India, where 70% of AWD cases had an acute abdomen.4,15,17,22 In these studies, viscus perforation from a variety of etiologies was the main contributor to acute abdomen. In the Addis Ababa, Ethiopia study, acute abdomen was the main contributing factor.2
Intestinal obstruction and acute appendicitis with its complications were the two most frequently performed procedures among the cases. In 57 cases (90.47%), the pathologies were benign. In contrast, a Sarajevo study discovered that the majority (40.1%) of abdominal wound dehiscence cases occurred following surgery for colorectal cancer and that 52.2% of all cases of abdominal wound dehiscence were malignant.16 84.9% of the patients in a Turkish study had undergone surgery for a malignancy.20 Our research shows that malignancy is much less frequent than benign pathologies, which may be because malignancy is uncommon in younger populations. However, due attention should also be paid to benign pathologies to minimize the development of abdominal wound dehiscence.
Our research also revealed that anemia was a significant risk factor for AWD. The odds of developing AWD were approximately four times higher in patients who had undergone laparotomy and had anemia than in patients who did not. This is supported by earlier comparable studies conducted elsewhere that show strong associations between anemia and wound dehiscence.11,15,16 But in another study done in Addis Ababa, Ethiopia no strong association was found between anemia and wound dehiscence.18
In this study 61(96.8%) of the cases had a long hospital stay compared to 44 (33.1%) of the controls. This is significant with a P-value of <0.001. This demonstrates how abdominal wound dehiscence increases a patient’s hospital stay with its associated consequences. This has been demonstrated in several studies. A case-control study conducted in Poland showed that the increased length of hospital stay among cases was statistically significant compared to controls .5,7 This was also demonstrated in a study conducted in Addis Ababa, Ethiopia.18
In the current study, majority (67%) of the wound dehiscences’ developed within 6 to 10 days of post laparotomy. The findings is in line with similar study conducted in addis ababa,Ethiopia revealing 58.5% of WD happened within similar time period.2 It is also similar with a study done in Pakistan.3 In a study done in Argentina majority of the cases occurred on the 9th post-operative day.10 According to Ramshort et.al 90% of cases of abdominal wound dehiscence occur before the 15th post-operative day.16
In this study, males (38 of 63, 60.3%) experienced abdominal wound dehiscence. Numerous studies have found that to be the case.2,3,15,16 In fact, age (being older) and sex (being a man) are two risk factors that are frequently mentioned in studies.10,11,19 In a study conducted in Addis Ababa, Ethiopia, there was no connection between sex and wound dehiscence.18 In our study, (44 out of 63, 69.8%) of the abdominal wound dehiscence cases were between the age of 15-61 years. This was comparable to the St. Paul, Ethiopia study.2 The same was the case with an Indian study.22 The high proportion of young people in the study population may be the cause of this. Similar research was conducted in India, where the majority of cases were in their fourth decade of life.15 In contrast, a study conducted in Sarajevo found that the majority of cases occurred in people between the ages of 71 and 80.16 In our study, only 5 (7.93%) of the cases were over the age of 61.
In contrast to some studies where the majority of the population was elderly, age and gender were not discovered in this study to be independent risk factors for the development of wound dehiscence. This was discovered in both an Egyptian and an Indian study.21,23 Age and gender were not found to have a statistically significant association in a case-control validation study carried out in Poland .5,7
Only 5 (7.9%) of the cases in this study had COPD, hypertension, or diabetes mellitus (DM) as comorbid conditions. This might be as a result of the higher percentage of young patients in this study than in other studies. As a result, these people have hardly any co-morbidities. COPD is one of the main independent risk factors documented in the literature.10,11 In contrast, a study conducted in Turkey found no evidence that COPD was significantly linked to the emergence of wound dehiscence.20
LIMITATIONS OF THE STUDY
It is challenging to extrapolate the study’s results to the country or the continent as a whole because it is facility-based and only includes two centers. Given that the secondary data were retrieved retrospectively from patient medical records, another limitation of the current study is the incompleteness of the records of some variables that might have an association with abdominal wound dehiscence and led to exclusion of them in regression analyses.
6. CONCLUSION
In this study, an AWD of 1.66 was found, and it was found that the patients’ place of residence, postoperative complications (SSI, anastomotic leak, HAP), anemia ,and emergency surgery, were all significant predictors of AWD development. We suggest giving patients from rural areas and those undergoing emergency surgery more attention. Prompt measures should be taken to prevent the development of postoperative complications; the root cause of anemia must be addressed whenever possible. Every patient’s medical history must be meticulously recorded.
7. RECOMMENDATIONS
This study is one of the few to evaluate the magnitude of abdominal wound dehiscence and its risk factors in the country. Future studies might involve many patients and multiple centers prospectively. This would make it possible to identify independent risk factors more precisely, allowing us to identify patients who are at a high risk of developing dehiscence and quickly take the necessary preventive actions.
ACKNOWLEDGMENTS
We are grateful for the opportunity to undertake this research, which was made possible by Hawassa University. The research directorate of Hawassa University College of Medicine and Health Sciences deserves special recognition for its remarkable collaboration. Last but not least, we would like to thank the data collectors, without whom the current data would not be feasible.