INTRODUCTION
The World Health Organization (WHO) reports that Five billion people globally lack access to surgical care, resulting in 18 million annual deaths and accounting for one-third of the global disease burden. In response, the WHO and its member states recognized surgical and anesthesia care as essential to Universal Health Coverage (UHC) in 2015.1 The Lancet Commission on Global Surgery (LCoGS) introduced the National Surgical, Obstetrics and Anesthesia Plans (NSOAPs) framework to guide countries in developing strategic plans for surgical systems. This framework has supported several low and middle-income countries (Zambia included) in strengthening emergency and essential surgical services as part of Universal Health Coverage (UHC) implementation.2 Defining essential surgical services is crucial for countries to provide comprehensive healthcare. NSOAPs play a vital role in integrating emergency and essential surgical care with other health services to achieve Universal Health Coverage (UHC) goals. Zambia was a pioneer in formulating NSOAPs in 2017, but implementation has been a significant challenge.3 Surgical care in Africa is predominantly centered in urban referral hospitals, leaving rural areas with limited access to quality surgical services. This disparity stems from a number of reasons including, Urban hospitals attract specialists due to better facilities, training opportunities, and living standards. Hospitals in cities have superior infrastructure, equipment, and resources. This has affected the rural hospitals negatively that it is difficulty to have access to essential surgical care in these remote areas.4 In several countries, district hospital-level surgery is almost exclusively provided by non-physician clinicians (NPCs), also called clinical officers, associate clinicians, or assistant medical officers. This is called ‘task shifting’.5 Compared to medical doctors, the duration of surgical training for NPCs is shorter (typically 2 to 3 years), with lower training costs and better retention rates. The term task-shifting applies, which the World Health Organization (WHO) defines as ‘the rational redistribution of tasks from highly qualified workers to health workers with shorter training and fewer qualifications’.6 In the case of surgery, it involves the delegation of surgical tasks from surgical specialists or general medical doctors (MDs) to surgically trained NCPs. The contribution to surgical care by the NCPs is often considered as a substitute for medically qualified professionals and concerns around the safety of surgical ‘task shifting’ solutions have been expressed. Research by Gajewski et al. found that NCPs in rural hospitals achieved comparable patient outcomes to medically qualified professionals measured by wound infections and surgical mortality. This study addresses concerns about ‘task shifting’ safety, suggesting that NCPs can effectively bridge the surgical workforce gap in the rural areas.7
It is known that even small facilities can deliver effective basic essential surgical services with careful utilization of the existing healthcare delivery structures already in use that can be leveraged to provide affordable and quality surgical care.8
MATERIALS AND METHODS
We conducted surgical camps across six districts at their hospitals. The local teams were informed at least two months before camp time. The communities were informed through radio announcements, posters, and messengers to clinics. The clinic staff then were made to spread the invitations to their catchment areas through community-based volunteers to the specific Neighborhood Health Committees (NHCs). The communities were asked to present themselves to the local facilities with all kinds of surgical diseases on the specified surgical camp dates. Patients who presented earlier than the surgical camp dates were accordingly booked for the camps.
All the camps had at least a Surgeon, a trainee Surgeon (or theatre nurse), and an anesthesia provider. The camps lasted on average five days with the daily work schedule of conducting ward rounds, outpatient screening, performing surgical procedures with the local teams, attending to all emergencies and holding clinical meetings. We looked at the booking lists and operation records for one-month period. Key members of staff (theatre nurses, anesthesia providers, medical licentiates, and Doctors) were interviewed using a google sheet designed questionnaire. We picked August of 2021 to analyze the type of operations done in the facilities as most of the citizens in region are farmers and it is assumed that by August, most of them would have less commitment to fieldwork and they would easily seek medical attention. This was also before the announcement of the surgical camps.
All patients who were seen during the camps by the surgical teams were recorded. Patients found with surgical diseases and fit for theatre were booked. We noted those who denied consent due to different reasons and those we referred for specialized investigations.
RESULTS
Analysis of records
No facility had booking lists for elective operations apart from those booked for the camps. The analyzed records reviewed a total of 299 operations done in the selected six hospitals. The majority of these operations were caesarian sections, at 68% followed by fracture manipulations at 13%. Hernia repairs were only done in one hospital, at 4% meanwhile exploratory laparotomies and excisions were both at 3%. See Figure 1.
Surgical camps
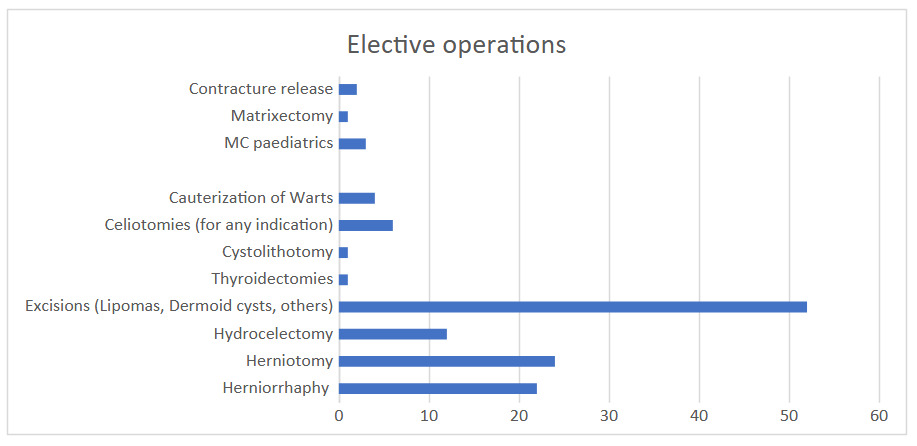
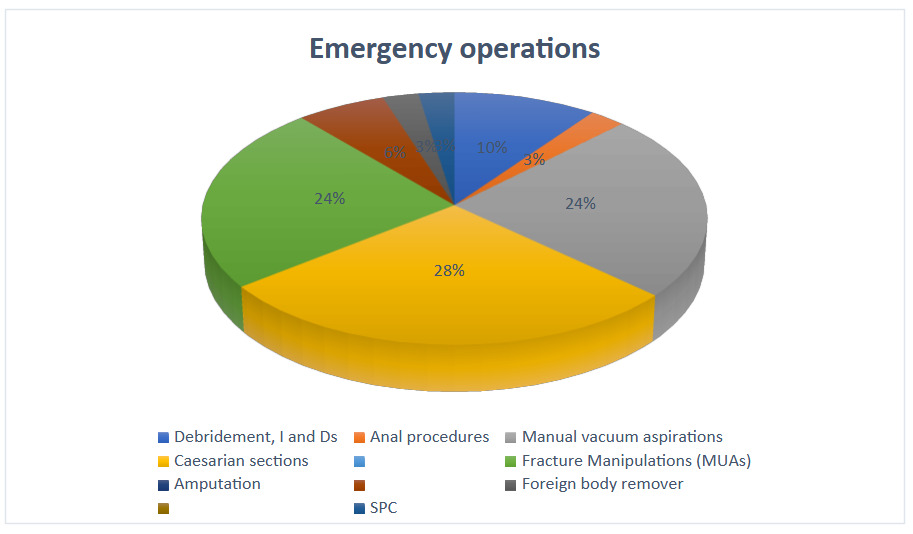
For our surgical camps, we screened 700 patients in total and operated on 219 different cases (Table 1). A majority of the patients (61%) operated on were over the age of 20 years (40% 20-39, 21% >40) with only 81 (39%) being <20. Those operated on were mostly males (57%) while females constituted 43%. Most cases for our camps were booked cases, about 65%. The majority of the emergency cases were obstetrics in nature (caesarian sections and post-abortal vacuum aspirations) at 53%. Of the elective cases, we had about 40% cases of inguinal hernia and 37% were lamps and bumps for excisions, Figures 2 and 3 have more details. Of note, 110 patients with clear surgical cases were not operated. Most of them did not show up (52%) due to their field/farm engagements or otherwise and 35% did not give consent while the rest (13%) were referred. A few were not operated due to a lack of basic investigations.
From the Interviews
We interviewed 32 members of staff. Ten barriers to surgery were given, as outlined in Table 2. Exhausted operating teams, unavailability of staff (Doctors and anesthesia providers), lack of surgical supplies and a lack of expertise were some of the most advanced challenges.
DISCUSSION
All anesthesia providers in the district hospitals are NCPs, mostly are former clinical officers or nurses. There is at least a medical licentiate (MLs) and medical officer (MO) at every facility. Not all theatres are run by trained theatre nurses. These are the cadres who do operations in the district hospitals with special emphasis on emergency obstetric cases. There are frequent refresher courses and mentorship programs for obstetric case management for these teams, but none of such programs are available for general surgical cases. Task shifting is very much being practiced but mostly on maternal and child health.9 Some facilities have no anesthesia providers and where available, it is only one provider per facility. The MOs and MLs have been made to give anesthesia in instances of unavailability of the anesthesia providers. This practice though risky, has been proven to be safe in resource limited settings.10 There is an imminent need to increase the numbers of all these cadres in the facilities across the region and frequent mentorships on other surgical conditions are also needed to improve care.11
The district hospitals by and large do obstetric operations, caesarian sections, and post abortal care, at 68%. As indicated by many authors12 and,13 obstetric emergencies are the main type of operations done in the District hospitals. The local teams are left exhausted by these cases and unable to go on with other surgical operations. During the study, fractures were the second leading emergency. In the Eastern province of Zambia, the simple fractures are managed by physiotherapists and all other fractures are referred to the next level of care. All district hospitals refer emergency general surgical cases to referral hospitals. Exhaustion, inadequate supply of consumables and a lack of experienced personnel are the major findings. With the district hospitals not doing elective operations patients with surgical conditions worsen or complicate. For Example, hernias have ended up being referred as complicated cases to the next level of care. This becomes a huge cost on both the healthcare system and the patient. There are patients who have also suffered socio-economic injustice due to inaccessibility of surgical care. For instance, the team operated on a man with a Hydrocele which had 2.7 liters of fluid, he was not able to socialize freely and was not economically productive for a long time. Lumps and bumps were the majority of elective cases we encountered but surprisingly, there were no records of these excisions being done in most hospitals. There are untold costs of referrals and morbidity plus mortality from these complicated cases that need to be assessed.
Among the poor staffing levels for the operating theatres, anesthesia providers are the least in the province. Some hospitals have no provider such that the teams are forced to learn how to provide lifesaving anesthesia only and refer the rest.14 In hospitals where only a single person is tasked to give anesthesia, there are reports of exhaustion and referrals become the rescue. There is a need to increase the recruitment of more medical doctors and anesthesia providers as a matter of urgency to all DHs. This may border on policymakers and politicians understanding the scope of this demand15 as this will increase the chances of achieving UHC.16 The main source of income for most people in the region is farming. This makes it difficult for these patients to leave the farm work and visit a health facility for most surgical diseases unless it is a debilitating condition. On the other hand, referral to the higher level of care is viewed costly as most of them cannot easily afford. The poor health seeking behavior is also in part due to poor education levels and has led to delayed presentations and poor outcomes. It is important to mention also that access to clinics and hospitals is not easy. People have to move long distances in order to find a facility. These reasons may have led to so many patients not showing up during the surgical camps. If it was possible, the best approach would be to operate on these patients immediately when they present without asking them to come back on an elective day because they are more likely not to show up. Poor infrastructure, inconsistent availability of medical and surgical supplies and in some cases, lack of surgical skills have also glossily attributed to poor surgical care in the province.
Zambia needs to invest in UHC with a holistic approach as recommended in the NSOAPs guidelines to improve surgical outcomes.2 We propose basic surgical operations, such as excisions of lumps and bumps, Hernia repairs, hydrocele surgeries, simple fracture management, amputations, Incisions and drainage of abscesses, and some emergency laparotomies to be offered in the district hospitals. This will demand for improved staff posting, skill enhancement among the local teams, infrastructure development as well as a consistent supply of consumables. Some of the neglected surgical cases in rural hospitals are hernias, skin excisions, hydroceles, burn management, and approaches to different emergency surgical cases. Short courses, such as basic surgical skills, basic non-operative fracture management, management of medical-surgical emergencies are highly recommended for all the critical health workers in rural hospitals.
Surgical camps and mentorship programs can also help to support the local teams with clearing booked cases and transfer of skills. However, this may be more costly than the other methods.
CONCLUSION
There is very little surgery being done in rural hospitals, as obstetric emergency cases have taken over the overstretched systems. The burden of surgery in rural communities is huge and the load is increasing every day. There is a need to bridge the gap so that we can take surgery closer to the communities where access will be easier and reduce the cost on both the patient and the health care system. Recruitment of more health workers, consistent supply of consumables, improvement of infrastructure, and skill enhancements will improve surgical outcomes.
Disclosure
This project was sponsored by the Royal College of Surgeons of Edinburgh (RCSEd) through the Fellowship of Remote Rural Humanitarian Healthcare (FRRHH). Funded the Surgical camps only