Introduction
Posttraumatic urethrospongiosum fistula is an acquired abnormal communication between the anterior urethra and the corpus spongiosum. Its occurrence is usually after traumatic catheterization but rarely occurs following penile trauma. According to a 2017 meta-analysis on the pattern of penile blood supply, about 61.9% are type 1 (only from internal pudendal artery), 32.8% type 2 (both from internal pudendal and accessory penile artery), and 5.4% type 3 (only from the accessory pudendal artery). Generally, variations of accessory pudendal artery are approximately 28.5%, mainly arising from the obturator artery, inferior vesical artery, and internal iliac artery, often on the left side supplying the penile part, which can result in significant blood loss if it is a fistula-feeding artery. However, due to the pendulous anatomical nature and its detumescence state in nonsexual excitation periods, the penis is less vulnerable to ordinary trauma. However, any penile trauma is a sensitive urologic emergency unless ruled out.1–3
Posttraumatic urethrospongiosum fistula is an extremely rare clinical condition. Particularly in conditions like accessory penile arterial supply to the corpus spongiosum, those arteries are highly likely to be the fistula-feeding artery, which leads to a high-flow pressure system with affected venous return. Because of the blood flow being redirected, this can cause a type of prolonged erection called nonischemic penile priapism, and it can sometimes lead to erectile dysfunction if the extra artery only supplies the corpus spongiosum. The patient presents with either erectile dysfunction late after the trauma incident or early with active bleeding per meatus. However, physicians usually attribute meatus bleeding following trauma to urethral injury, and it may be overlooked and delay diagnosis.4–6
Diagnosis of posttraumatic urethrospongiosum fistula needs a thorough history and physical examination; the mechanism of trauma is particularly crucial, and cystoscopic examination has an important diagnostic and therapeutic role. In resource-limited areas, Doppler ultrasound is sensitive and helpful in making diagnoses. In an ideal setup, digital subtraction penile angiography is a confirmatory test.7,8
Surgical management options depend on medical setup and surgical experience. In an ideal setup, endoscopic-guided, highly selective, and super selective penile arterial embolization is the best treatment choice. However, in places where resources are limited, open surgical ligation of the fistula-feeding artery is a treatment option with comparable outcomes.9–11
Case Description
History and physical examination
A 70-year-old male patient presented with continuous bright red bleeding per meatus of 1 day’s duration. He sustained a sudden horse kick to his perineum 3 days prior but had no difficulty urinating, and he denied the incident was related to a sexual act. Otherwise, he had no prior history of surgery or chronic illness. There was no history of any catheterization trial from the referring hospital.
Upon objective physical examination, he was acutely sick-looking and had an active bleeding from the meatus. Vital signs were heart rate at 90–110 beats/min and blood pressure at 118/71 to 109/65 mmHg). Pertinent positive findings were found upon head, eyes, ears, nose, and throat (HEENT) examination: pale conjunctiva and nonicteric sclera. Genitourinary system (GUS) examination included no costovertebral angle tenderness, blood-soaked perineal underwear cloth, active bleeding from flaccid penile meatus, palpable testicles, and no gross penile deformity/wound noticed.
Investigations
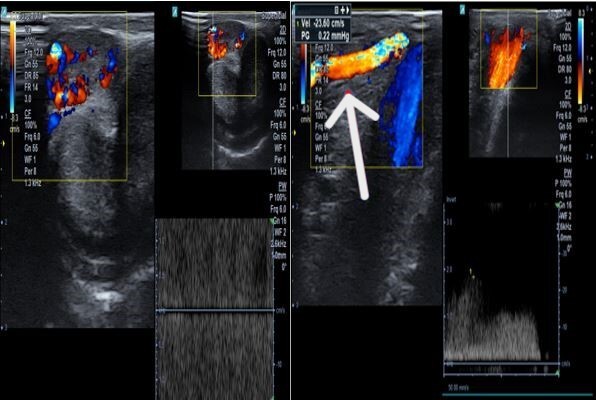
The patient was investigated with an initial impression of posttraumatic anterior urethral injury. Complete blood count showed serial hemoglobin: Hgb-12.1g/dL from the referring hospital and Hgb-9.3g/dL initially, which then dropped to Hgb-6.2g/dL. Penile and scrotal Doppler ultrasound (Figures 1 and 2) found an 8 mm by 5 mm right side accessory artery arises from the external iliac/external pudendal artery with high flow directly communicating to the penile corpus spongiosum body. Otherwise, there was normal anatomy of corpora cavernosa and tunica albuginea and mild scrotal edema. The patient underwent a diagnostic cystoscopic examination, which found an actively bleeding vessel with bulged urethral mucosa at the right side distal to the fossa navicularis and no evidence of urethral injury (see Video 1).
Management outcome and follow-ups
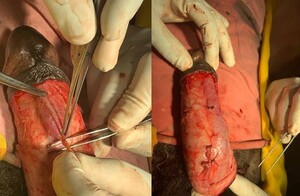
With a final diagnosis of posttraumatic distal penile urethrospongiosum fistula, the patient was counseled for open ligation. The patient underwent open penile exploration layer by layer. The accessory penile artery with distal branch supplies the distal spongiosum body (Figure 3). Tunica albuginea and corporal bodies were grossly intact. The accessory penile artery was identified and ligated (Figure 4), and penile tissue was closed in layers. Postoperatively, no bleeding from the fistula site was observed on cystoscopic examination, and the control Doppler ultrasound was unremarkable. The patient was much improved and discharged. The patient had no urinary complaints and normal penile Doppler ultrasound findings on subsequent follow-ups at 1, 2, and 3 months.
Discussions
Urethrospongiosum fistula is an acquired abnormal communication between the penile urethra and the corpus spongiosum body. However, the corpus spongiosum is supplied by the bulbourethral artery; it does not directly involve erectile penile function. Rather, it is the imbalance of blood supply and venous return that affects penile tumescence due to shunt.4,5
The most common causes for clinical presenting symptoms of urethrospongiosum fistula described in the literature are bleeding and urine extravasation in corpus spongiosum space. However, when the fistula-feeding artery directly communicates with the corpus spongiosum urethral mucosal epithelium, the patient can present with active meatal bleeding, which is an extremely rare clinical condition.6
Diagnosis is based on clinical history, physical examination, and penile imaging. Doppler ultrasound is the most sensitive and convenient imaging modality in resource-limited areas for diagnosis and follow-up as well. On ultrasound, a high-pressure flow of the feeding artery, a dilated and thick wall of the draining vein, and high-velocity turbulent flows are the main indicators of acquired arteriovenous malformation.4,7,12
However, computed angiography and magnetic resonance are the choices of imaging, particularly in trauma-related pelvic injury. On computed angiograms, early enhancement of the fistula draining vein is seen from an enhanced arterial phase and filling of the adjacent vein.8,13
On the other hand, the most advanced and accurate form of imaging is digital subtraction angiography, which shows nearly perfect anatomy in a sequential manner and enables direct localization of the fistula-feeding artery in complex arteriovenous, arteriocavernosal, and urethrospongiosum fistulas. However, digital subtraction angiography is an invasive procedure that needs an experienced hand and is often available in an ideal setup.9
The goal of surgical management in penile urethrospongiosum fistula is to ligate/embolize the feeding artery and draining vein in arteriovenous malformation. On the other hand, closure of the proximal feeding artery may be enough in arteriocavernosal and urethrospongiosum fistulas. The choice of management depends on specific diagnosis, professional expert preference, and material availability in the setup. As described in the literature, endovascular embolization is more ideal in complex fistulas compared to open ligation. Techniques of endovascular treatment are either autologous blood clot or chemical agents. Overall success rate reached more than 89%.10,13,14
Even though there are limited case reports in the literature regarding postoperative outcomes and expected postoperative complications after selective embolization of a posttraumatic urethrospongiosal fistula, we found 2 reported cases as per our search knowledge. Both patients were treated with endovascular embolization, and erectile function was restored successfully on 6-month follow-up. However, in our case, we treated with open ligation of the proximal feeding artery.
Conclusion
For a patient with meatus bleeding following blunt perineal trauma, urethrospongiosum fistula with a rare variety of accessory penile arterial supply should be a differential diagnosis. Doppler ultrasound combined with cystoscopy is a helpful diagnostic tool in resource-limited areas. In an ideal setup, angioembolization is the best treatment. However, open ligation of the fistula-feeding artery is an effective management option in our setups with a satisfactory outcome.
Acknowledgments
We would like to express our gratitude to the patient for providing informed consent for publication along with accompanying image as well as everyone else who helped with the intraoperative photo and radiologic image collection.
Ethical Approval/Informed Consent
Formal ethical approval was not required for this case report as per institutional guidelines/local regulations for retrospective reporting of a single clinical case. Formal written, informed consent was received from the patient along with accompanying images. Any identifying part has been anonymized for the privacy and confidentiality of the patient.
Data Availability
Not Applicable
Conflict of Interest
No conflict of interest in computation.
Funding
None


_accessary_p.jpeg)

_accessary_p.jpeg)
