Background
Familial adenomatous polyposis (FAP) results from a mutation of the APC gene, an autosomal dominant syndrome with 100% penetrance for colorectal cancer.1 FAP phenotypically is associated with Gardner syndrome, Turcot syndromes, and attenuated adenomatous polyposis coli.
FAP is the second most common inherited polyposis syndrome with a birth incidence of about 1 in 8300. 70% of patients have a known family history with an equal male-to-female ratio with the remaining 30% having a spontaneous incidence with no identifiable family history.
Data on FAP in Sub-Saharan Africa are scarce, with only a few case reports documented in countries like The Democratic Republic of Congo, Uganda, and Nigeria.2,3 Reported cases include 2 middle-aged men in Nigeria, both in their 40s, who exhibited symptoms of dull abdominal pain and hematochezia. Another case involved a 12-year-old boy in Goma, DR Congo, with a similar clinical presentation. The colonoscopies in all 3 patients revealed polyposis. One of the Nigerian patients was diagnosed with metastatic adenocarcinoma involving the peritoneum and received palliative chemotherapy, while the other 2 underwent prophylactic colectomies.
If affected individuals are not treated, they usually develop hundreds of colorectal polyps, which generally manifests in teenage years. The continued development of the colorectal polyps predisposes them to a 100% colorectal cancer risk by the age of 50. A total colectomy is usually the treatment of choice to significantly reduce the risk of developing colorectal cancer. Patients also have a high risk of developing other malignancies such as, gastric and duodenal adenocarcinoma, hepatoblastoma, and desmoid tumors.1,4
Case Presentation
The 35-year-old male’s medical history included a 5-year history of intermittent hematochezia, occasional colicky lower abdominal pain, and progressive weight loss. He had been using peptic ulcer medications with no symptom relief. In early 2024, his symptoms worsened, prompting him to seek care at our referral facility. On examination, he had a lean body mass, multiple rectal polyps on digital rectal examination, and a scaphoid abdomen without palpable masses or tenderness.
The colonoscopy (Figure 1) revealed extensive proctocolic polyposis, with histology confirming tubular adenoma. The staging CT (Figure 2) identified multiple focal polypoid lesions in the anal canal and proximal sigmoid colon, the largest measuring approximately 2.58 cm in maximal thickness. The chest CT was normal. Given these findings, a multidisciplinary team (MDT) recommended proctocolectomy with abdominoperineal resection (APR) and terminal ileostomy.
The patient had an uneventful recovery after the procedure, and he was discharged after 1 week. Histopathological analysis of the specimen confirmed the presence of over 100 proctocolic polyps, the largest measuring 5 cm, with moderately differentiated adenocarcinoma affecting multiple sites, primarily the rectum. Margins were negative for invasive tumors.
Two months postoperatively, the patient developed obstipation and bilious vomiting and was diagnosed with small bowel obstruction due to adhesions. He was managed nonoperatively. He improved and was discharged. He is scheduled for an upper GI endoscopy and further MDT discussion.
His 42-year-old sister was diagnosed with FAP following a colonoscopy that revealed proctocolic polyposis with tissue histology showing tubular and tubulovillous adenomas. She underwent pancolectomy with ileal pouch formation in November 2023. She had an uneventful recovery, and she was discharged after 1 week. Histology showed over 100 high-grade tubulovillous adenomas with no stromal invasion. However, in September 2024, she presented symptoms of gastric outlet obstruction, dehydration, and acute kidney injury. An upper GI endoscopy revealed multiple duodenal polyps. A laparotomy found a restrictive band in the fourth part of the duodenum with proximal dilatation and multiple small bowel adhesions. Adhesiolysis and band release were performed, followed by gastrojejunostomy with jejunojejunal Braun anastomosis. She initially recovered well, but was readmitted 2 weeks later with persistent postprandial bilious vomiting. Her follow-up upper GI studies were essentially normal, but she was unable to recover and passed due to worsening symptoms.
The patient’s other 4 siblings (2 sisters and 2 brothers) have no current health concerns but have not undergone colonoscopy screenings or genetic testing. His mother is alive and well. His father passed away at 33 from colon cancer. Two paternal uncles passed away from colon cancer in their 30s and 40s, while another uncle passed away in his 40s from severe diarrheal disease.
The 33-year-old male with a five month history of an enlarging perianal mass, started initially as a small nodule and was treated as a perianal wart with podophyllin. The mass ulcerated, began discharging mucoid fluid, and progressively increased in size. This caused dull perianal pain which was relieved by ibuprofen.
On examination, the patient was in good general condition. Digital rectal examination revealed a fungating, mucoid producing perianal mass measuring approximately 6 × 3 cm at the 1 to 3 o’clock position, with an ulcer extending into the anal canal at the 3 o’clock position (Figure 3).
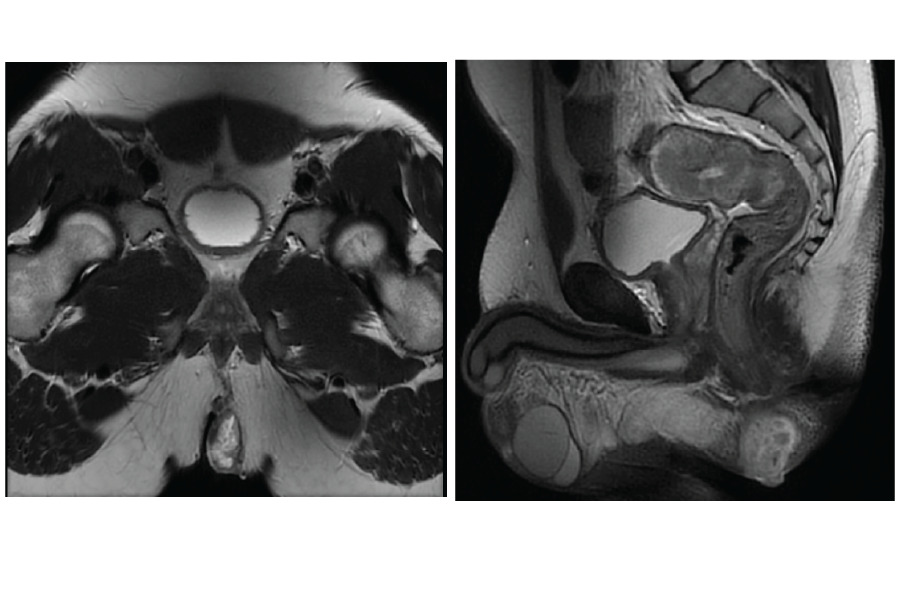
The colonoscopy (Figure 4) revealed proctocolic polyposis involving the anal canal. A polypectomy was performed, and the tissue histology confirmed benign tubulovillous adenoma. Examination under anesthesia and biopsy 3 weeks later yielded similar histological findings. A pelvic MRI (Figure 5) demonstrated a perianal mass with an extrasphincteric fistula approximately 4 cm from the anal verge.
The patient was initially reluctant to undergo surgery but consented after multiple counselling sessions and MDT discussions. He was admitted 8 months later and underwent laparoscopic APR. His postoperative course was uneventful, and he was discharged after 10 days (Figure 6). The study of the tissue histology confirmed mucinous adenocarcinoma.
The patient has no known family history of colorectal cancer. He is the firstborn in a family of 4, and both his parents and siblings are alive and asymptomatic. No screenings of his family have currently been conducted.
Discussion
FAP usually forms with more than 100 colorectal polyps. If the colorectal polyps are untreated with a prophylactic proctocolectomy procedure, there is a 100 penetrance for colorectal cancer by the age of 50.
It commonly occurs with extracolonic manifestations including osteomas, desmoid tumors, thyroid tumors, ondontomas, sebaceous cysts, periampullary tumors, and congenital hypertrophy of retinal epithelium.5 A milder form, Attenuated FAP which also results from APC gene mutation, occurs at distinct codons and is typically accompanied with fewer polyps, a late onset, and a slower progression to cancer development.
The APC gene is typically a tumor suppressor, but when mutated, it disrupts apoptosis, resulting in uncontrolled cell growth. This makes the mutated APC gene a precursor for adenoma development in FAP.
Screening usually includes annual or biennial flexible sigmoidoscopy or genetic testing for high-risk family members from age 10 to 12 years. Endoscopy of the upper GI should also be performed to rule out concomitant upper GI polyps because there is a high likelihood of coexisting syndromes.
Nonsteroidal anti-inflammatory drugs like sulindac and selective cyclooxygenase-2 (COX-2) inhibitors are used as chemo-preventive drugs and have been shown to reduce the number and size of polyps in individuals with FAP.6
Definitive treatment usually involves proctocolectomy with ileal pouch-anal anastomosis or end ileostomy, which provides the highest chances of getting rid of susceptible colorectal mucosa. Pancolectomy with ileorectal anastomosis preserves the rectum and is less extensive, but individuals require endoscopic evaluation every 3 to 6 months.
After colectomy, cancer risk persists in residual anorectal tissue in ileal-pouch-anal anastomosis or terminal ileal stoma in APR, necessitating endoscopic surveillance every 6 to 12 months or annually, respectively.7,8 There is a 45% adenoma9 risk at 10 years and a 1% risk of adenocarcinoma risk in the ileal pouch.10 Pouchitis may occur in 22% of patients, especially those with a history of irritable bowel syndrome.11
Conclusion
Data on FAP in Sub-Saharan Africa are limited with inadequate screening programs. Therefore, national governments need to adopt targeted screening, especially for first-degree relatives of early-onset colorectal cancer patients, to enable early detection and intervention.
Acknowledgment
I would like to acknowledge the 3 patients for giving consent to have their cases published.
Informed Consent/Ethical Approval
Formal ethical approval was not required for this case report as per institutional guidelines/local regulations for retrospective reporting of a single clinical case. Written consent for submission and publication of this case including imaging and associated text has been obtained from the three patients in line with COPE guidelines. Patient anonymity was maintained throughout the report by de-identifying all patient data.
Data Availability
Not applicable
Funding
None
Conflict of Interest
The authors declare no conflict of interest.





_of_the_tumor.png)




_of_the_tumor.png)