Introduction
The global health sector has made enormous strides in safety, technology, and efficiency. However, with these advancements, the environmental sustainability of current surgical practices is increasingly under scrutiny. One area of concern is the widespread use of disposable plastic instruments and supplies in operating theaters (OTs), particularly in high-income countries.
Historical and Global Practices: Reusables vs. Disposables
Historically, reusable cotton and polyester-cotton blend fabrics were standard for surgical gowns and drapes. These materials evolved to include water-repellent finishes to enhance barrier protection. In many low-resource settings, reusable cloth drapes, gowns, and metal instruments are still the norm as reprocessing through sterilization allows for repeated use. Conversely, in developed countries, there is near-universal reliance on single-use, plastic-based products.
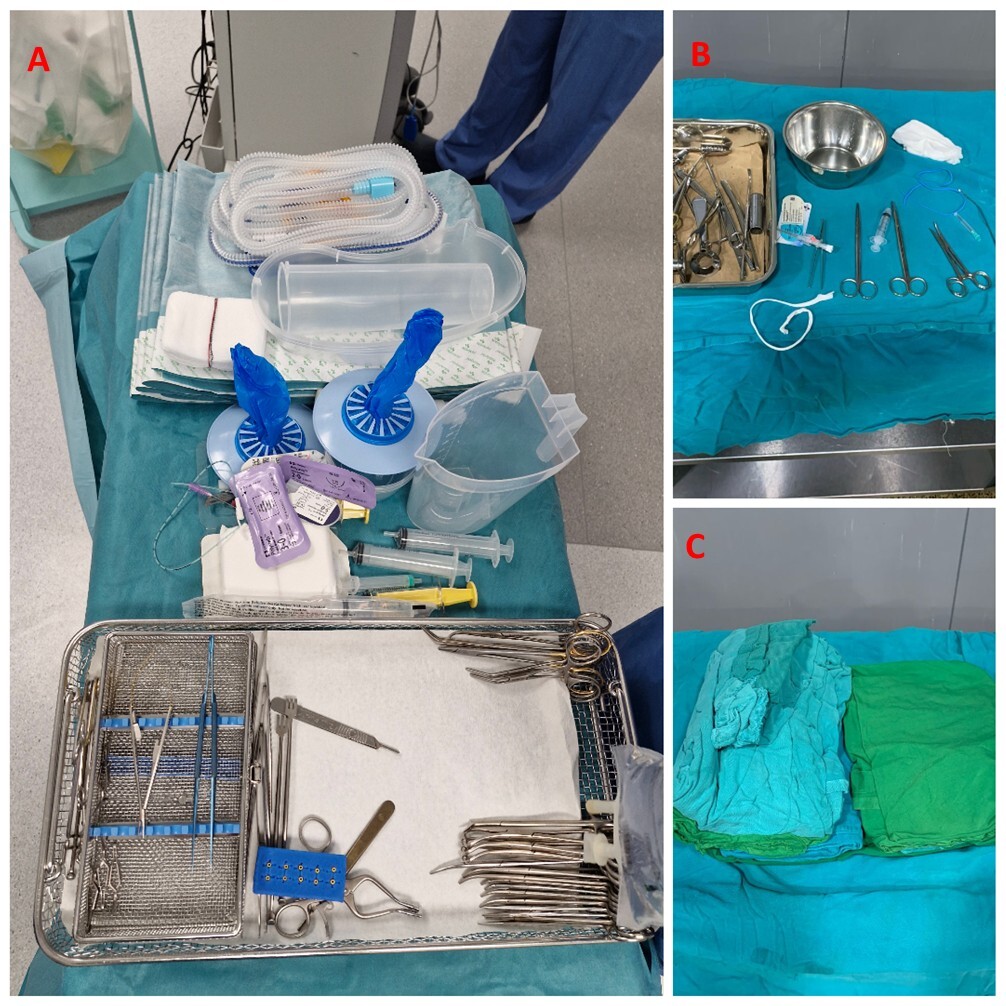
As illustrated in Figure 1, there is a stark contrast between surgical setups in different contexts. Figure 1A depicts a typical surgical tray from a UK operating theater, featuring numerous disposable plastic items, including single-use drapes and light handle covers, underscoring the heavy reliance on plastics in high-income settings. In contrast, Figures 1B and 1C show surgical trays from a sub-Saharan African country where reusable cloth gowns, drapes, and metal instruments predominate. These items are routinely sterilized and reused, exemplifying a more sustainable practice that has been largely abandoned in wealthier health care systems. This visual comparison highlights the need to reconsider current practices in developed countries and explore the potential for reintegrating reusable surgical materials without compromising safety.
Environmental and Economic Costs of Disposables
The environmental cost of this shift is significant. In the United Kingdom, the National Health Service generated over 408,000 tons of waste in 2005–2006, with 29% classified as clinical waste and an annual disposal cost of nearly £73 million. This amounts to 5.5 kg of waste per patient per day, much of it from disposable plastic items used in surgery.1 Fear of infection transmission has driven the preference for disposables, yet this may be addressed with robust sterilization protocols for reusables.
The literature on infection rates comparing reusable and single-use gowns and drapes is inconsistent. Earlier studies often suffered from methodological flaws, including lack of randomization, inadequate product descriptions, and biased outcome assessments.2 More recent systematic reviews highlight the urgent need for high-quality, multicentre research to evaluate both environmental and clinical outcomes.3,4
The health care sector contributes an estimated 4.4% of global greenhouse gas emissions.5 In the United Kingdom alone, the National Health Service accounts for 5.4% of national emissions, with surgical instrument procurement representing 13.2% of that total.3 Alarmingly, the production and disposal of plastic are expected to generate up to 2.8 gigatons of green house gases annually by 2040.6 OTs are particularly resource-intensive, producing up to 814 kg of CO₂-equivalent emissions per operation—comparable to driving 3650 km in a gas-powered car.7
Waste Management and Recycling Challenges
Recycling rates in the United States have steadily improved, rising from 16% in 1990 to nearly 35% by 2011. Despite this progress, health care facilities remain the second largest source of waste nationally, generating more than 4 billion tons each year. Studies from individual hospitals suggest that over half of operating room waste is clean and could be recycled, yet it is often misclassified as hazardous. This mismanagement is largely attributed to inadequate staff training on waste segregation and limited awareness of the cost implications of improper disposal.8
Initiatives for Sustainable Surgery
There is a pressing need to reassess the environmental sustainability of surgical practices. Initiatives such as “green operating theaters” promote reduced water use (eg, alcohol-based surgical scrubs), waste segregation, staff education, and behavior change to minimize ecological impact.4,9 Many disposables, including packaging, are incorrectly classified as clinical waste, increasing disposal costs up to 20-fold and reducing recycling potential.10
Developed countries must re-evaluate their current reliance on single-use items. Reintroducing reusable alternatives—supported by strict sterilization protocols and monitored life cycles—could substantially reduce waste without compromising patient safety. Policies must weigh environmental, clinical, and economic outcomes holistically.
Perspectives from Low- and Middle-Income Countries
Evidence from sub-Saharan Africa remains scarce regarding the environmental impact of disposable surgical items and their contribution to carbon emissions. However, a descriptive study from 3 referral hospitals in Kigali, Rwanda, highlights the broader challenges of medical waste management in OTs. The study found that although knowledge (54%) and practice (55%) among theater staff were rated as relatively good, major barriers included lack of equipment (71%), negligence (66%), and inadequate training (57%). These findings underscore that beyond the global debate on disposables vs reusables, structural limitations such as inadequate systems, policies, and resources strongly influence waste practices in low- and middle-income countries (LMICs). This gap illustrates the need for region-specific data and tailored strategies rather than reliance solely on evidence from high-income countries.11
In conclusion, surgical sustainability requires coordinated efforts from policymakers, clinicians, and hospital leadership. We call for rigorous, multicentre studies comparing the life-cycle impacts of disposable and reusable surgical products, and urge health care systems in high-income countries to consider evidence-based re-adoption of sustainable practices still prevalent in many low-resource settings.
Expert Opinion
It is essential to consider the broader implications of surgical practices on environmental sustainability, particularly in LMICs. Resource limitations often necessitate the reuse of surgical items, but many LMICs have yet to systematically integrate environmentally friendly approaches into OTs and hospital-wide waste management systems. Future developments should focus on creating theater environments that balance environmental responsibility with stringent patient safety standards, particularly regarding infection control and sterility.
Further research is needed to quantify and compare greenhouse gas emissions and the economic burden associated with single-use, high-waste systems in developed countries vs predominantly reusable systems in LMICs. Such studies would inform evidence-based policies that optimize both ecological sustainability and clinical outcomes. Building environmentally conscious health care systems in LMICs could not only reduce waste but also serve as a model for sustainable surgical practice globally.
Data Availability
Not applicable
Conflict of Interest
The author(s) declare they have no competing interests.
Funding
No funding or grant support.