Introduction
Hypospadias is an arrest in the normal growth of the ventral, foreskin, and urethral aspects of the penis.1 It is the second most common anomaly after undescended testes, with an estimated prevalence of 1 in 200 boys.2 Hypospadias is classified based on the positioning of the urethral meatus, ie, proximally, midshaft, or distally located.2 There is a wide variation in reported complication rates after hypospadias surgery, which is between 5%–70 % in the published literature. This variance is compounded by differences in reporting and follow-up.3,4 These complications are graded based on the necessity for an additional surgery on both functional and cosmetic parameters.5,6 Notably, a single reoperation increases the risk for additional complications by 20%; likewise, a second reoperation or more increases the risk to 40%.7 Re-operative surgery in hypospadias is generally associated with increased morbidity, prolonged hospital stays, increased hospital costs, and patient dissatisfaction.8
The aim of this study was to determine the outcome of re-operative surgery in patients after primary hypospadias repair.
Materials and Methods
Study design
This was a retrospective study of patients diagnosed with hypospadias from January 2013–December 2022. The study was carried out in Kenyatta National Hospital (KNH), which is a referral facility for pediatrics urology patients in Kenya.
Study population
The study population included all patients diagnosed with hypospadias who underwent primary hypospadias repair at KNH from January 2013–December 2022.
Sample size determination
Sample size estimation was calculated using a statistical Cochrane formula: N = Z2 [P(P − l)] D2.
Where
Z2 = Standard error associated with chosen significance level (1.96).
D2 = sampling error margin (0.05).
P = prevalence of reoperation; the expected P is 0.15% (15).
N = Sample size.
N = 1.96 x 1.96 [0.15 (1 – 0.15)] (0.05)2 = 168
Inclusion criteria
We included all pediatric patients diagnosed with hypospadias who underwent primary repair at KNH, with a follow-up period of more than 6 months since the first salvage procedure.
Exclusion criteria
We excluded all patients with incomplete records and all patients whose first salvage procedure was done at another facility.
Data collection
Patients’ records were retrieved electronically; data on rates, indication, and outcomes of re-operative surgery were collected with a follow-up period of 6 months. The principal investigator was responsible for data collection, assisted by 2 research assistants.
Data management and analysis
Patient identifier numbers were assigned to patients’ records for confidentiality purposes. Hard copies of the data were kept in a lockable cupboard within the hospital premises, and computed data was stored in a password-secured folder to prevent unauthorized access. The outcome measures included occurrence of previous complications requiring salvage surgery, occurrence of new complication requiring salvage surgery, and the number of additional salvage procedures performed. Outcome also measured the average length of stay and the average cost of treatment. Descriptive data were analyzed based on frequencies, proportions, and measures of central tendency, ie, mean, median, S.D., and interquartile range measures.
Ethical consideration
This study was approved by the institutions’ ethics and research committee (KNH/UON-ERC, REF No. P503/052023)
Results
This study investigated the reoperation rates in hypospadias, the indications, and the outcomes of reoperation in 159 patients who underwent primary hypospadias repair at KNH.
Demographic and clinical characteristics
The mean age at diagnosis was 4.7 years, and age at repair was 4.9 years (Table 1). The incidence of failed primary repair was 66/159 (41.5% [CI 33.9−49.2]).
Indication for re-operative surgery
The most common indication for surgery after failed primary repair was occurrence of Urethrocutaneous fistula in 40 patients (Table 2).
Outcomes of reoperation after failed hypospadias surgery
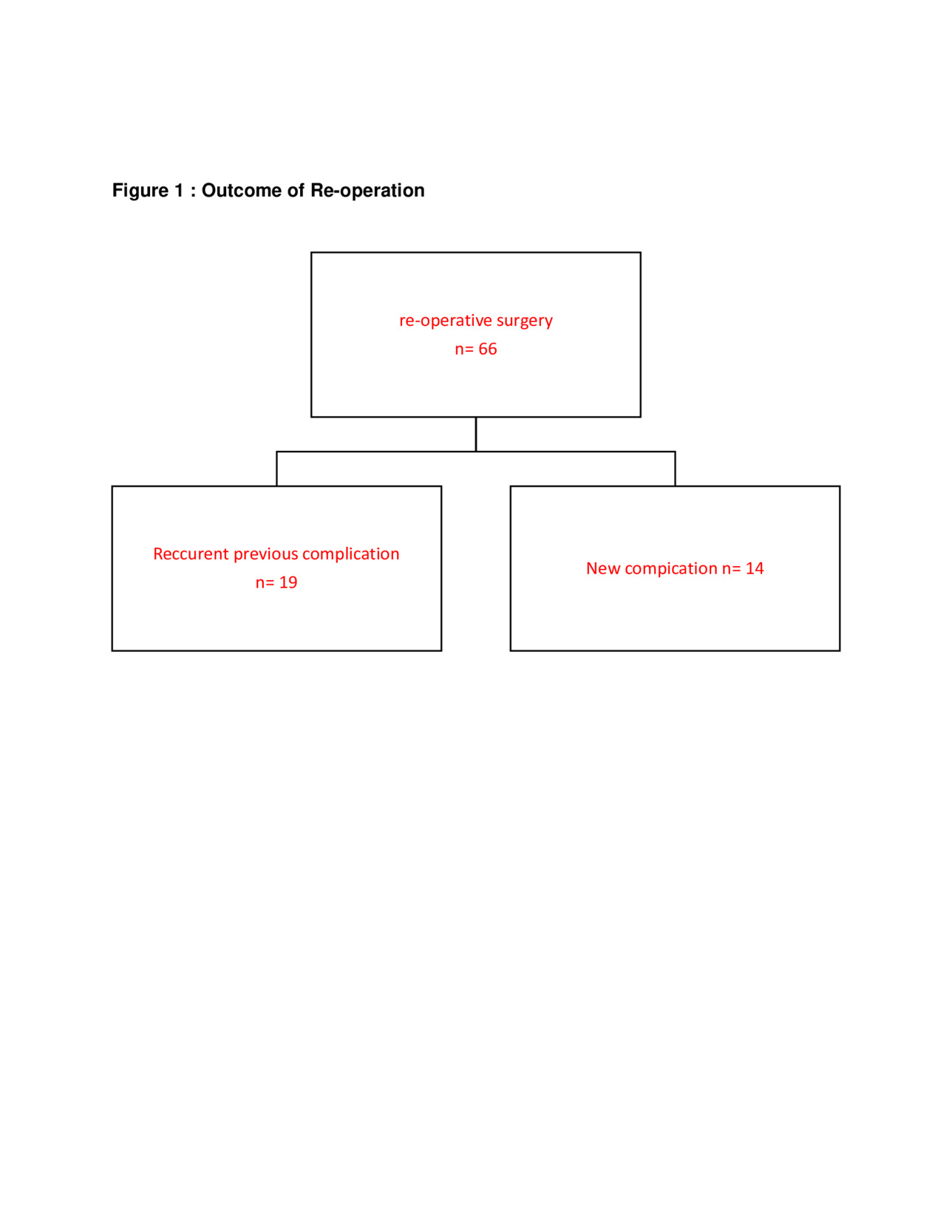
Of the 66 patients who underwent re-operative surgery, 19 (28.8%) had recurrence of the previous complication. Specifically, 13 (19.7%) had recurrence of urethrocutaneous fistula, 2 had recurrent chordee, urethral stricture recurred in 2 patients, with meatal stenosis recurring in 2 patients. One patient had both meatal stenosis and urethral stricture (Figure 1).
After salvage surgery, 14/66 (21.2%) patients had a new complication. Of these patients, the complications included meatal stenosis 3, urethrocutaneous fistula 6, complete breakdown in 3, partial breakdown in 1, and urethral stricture in 1 patient (Figure 2).
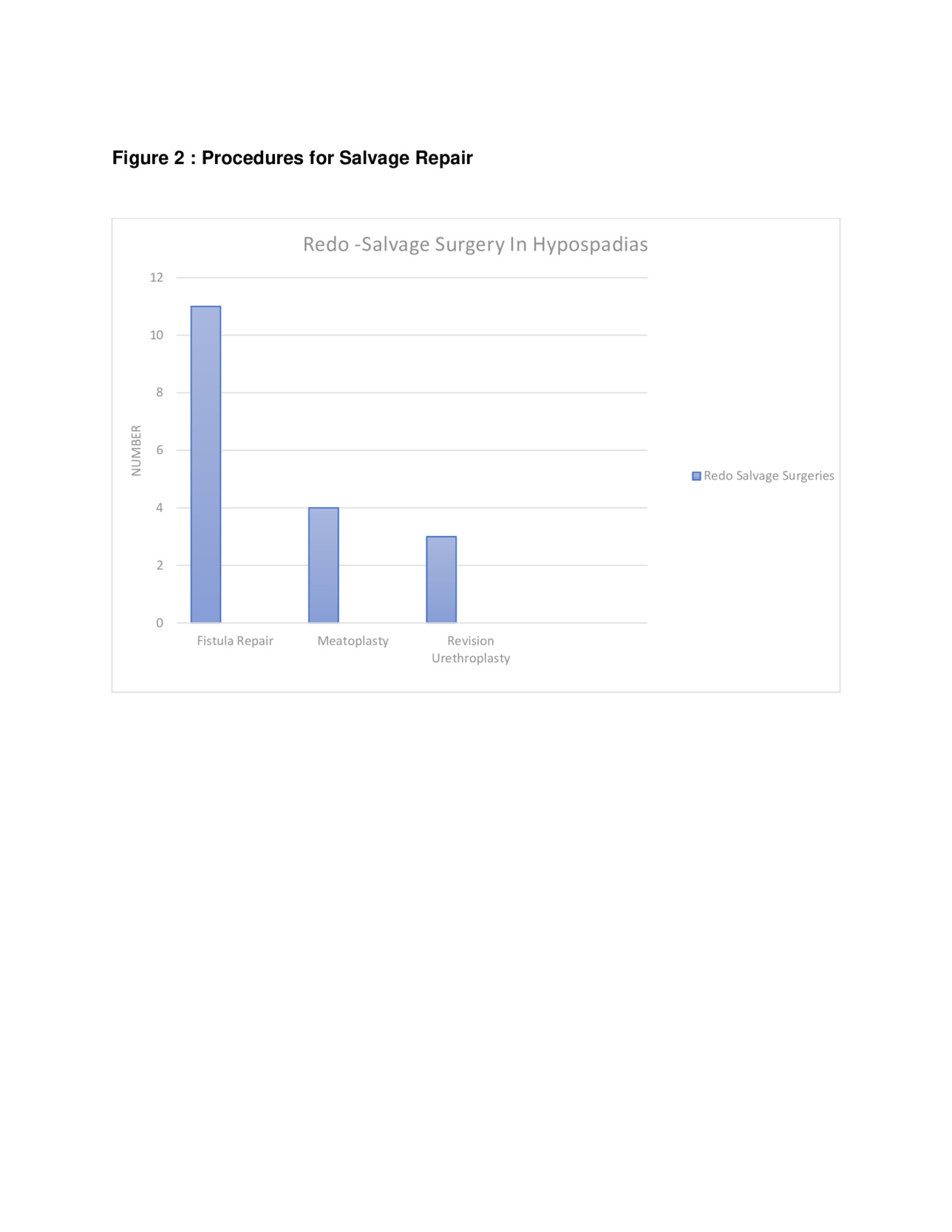
After initial salvage procedures, 18 patients needed a further salvage procedure, where 13 patients needed just 1 procedure, 3 needed 2 procedures, 1 patient needed 3 procedures, and an additional 1 patient needed 4 procedures. Specifically, Urethrocutaneous repair was the most common additional salvage procedure in 11 patients, followed by meatoplasty in 4 patients and tubularized incised plate (TIP) repair in 3 patients. The distribution of complications differed significantly within both one-stage (χ² = 88.91, P < 0.001) and two-stage (χ² = 32.00, P < 0.001) repair groups, indicating that urethrocutaneous fistula was the most common indication for reoperation (Figure 3). The Length of stay and hospital-related costs are presented in Table 3.
Discussion
This study investigated the outcomes of re-operative surgery following failed primary hypospadias repair. The study adds to the pool of data on reoperations after initial hypospadias repairs, which is essential for improving surgical outcomes and patient care. A total of 159 patients were included.
The study found a significant failure rate of re-operative surgery coupled with a significant increase in health care-related costs. In regions with limited health care resources, such as Kenya and other low- to middle-income countries, the repeated cost of surgeries—along with indirect costs such as travel, lost wages, and time away from school—compounds the financial strain on families. The findings provide critical insights into both the post-surgical challenges and successes at KNH for both care providers and the patient.
The research highlights that the most common primary repair technique was the TIP procedure, performed in 51.6% of cases due to its low complication rate, favorable cosmetic outcome, and simplicity. The most common location of hypospadias in this study was subcoronal, accounting for 34.6% of cases, followed closely by penoscrotal hypospadias at 33.3%. Perineal hypospadias was the least common, occurring in only 0.6% of patients. This was consistent with research done by JK Kamwetu (2020) at KNH, where he reveals the subcoronal 24 (47.1%), followed by penoscrotal 11 (21.6%). This is also consistent with global findings, where studies often report the subcoronal as the frequent location of hypospadias.2,5,9–11
In our research, the average age of hypospadias repair was 6.4 years. This is similar to the age of repair in South Africa and other African countries.12 However, the age at which hypospadias repair is performed varies globally, influenced by health care resources, surgical training availability, and cultural factors. In North America, most children undergo initial hypospadias repair within the first 2 years, a practice supported by research linking younger age with fewer complications. European practices are similar but extend the window slightly, with most surgeries occurring within the first 3 years. In China, however, the average age at repair tends to be later, often within the first 5 years.11
The incidence of failed primary repair was 41.5%, significantly higher than reported in studies from Egypt (15%) and Nigeria (12%).12,13 In terms of reoperation rates by hypospadias location, data from the Association of American Medical Colleges over 9–10 years reported secondary surgery rates of 12.6% for distal, 13.9% for proximal, and 46.6% for perineal hypospadias. However, our study revealed significantly higher rates, with secondary surgeries occurring in 49% of patients with subcoronal hypospadias, 27% with mid-penile hypospadias, and 47% with penoscrotal hypospadias.
The study revealed that the most common indication for reoperation after failed primary hypospadias repair was the development of urethrocutaneous fistula, which occurred in 36 patients (54.6%). This was followed by complete breakdown of the repairs in 8 patients (12.1%). Notably, 90% of the fistulas occurred as single fistulas in the subcoronal region, the same location as the abnormal urethral opening. These findings align with other studies, such as the Tanzanian study by Mteta et al, which reported urethrocutaneous fistula as the most frequent long-term complication of hypospadias repair, with a 40.5% prevalence. Similarly, Waleed et al found that urethrocutaneous fistula accounted for 25% of reoperation cases.13,14 This pattern is also consistent with studies conducted in Nigeria and Kenya. In Nigeria, there was a reported urethrocutaneous fistula rate of 38% of patients, while in Kenya, a similar study found a urethrocutaneous fistula rate of 47% of patients.15 A French study further supported these findings, reporting a 36.2% overall incidence of long-term complications, with fistulas accounting for 12.9%. However, a study in Egypt differed, finding meatal stenosis to be the most common indication for re-operative surgery post-hypospadias repair. These variations in complications and indications for reoperation underscore regional differences and the complex nature of hypospadias surgery outcomes.12,13,15,16
In evaluating the outcomes of re-operative procedures following failed primary hypospadias repair, it was found that out of 66 patients who underwent salvage surgery, 18 (27.7%) required an additional reoperation, a rate consistent with findings from Snodgrass and Lorenzo (20%) and Tarek et al in Egypt (23.8%).17,18 A separate study in Iraq showed a high success rate with dilation in re-operated patients.19 Recurrence of the initial complication, primarily urethrocutaneous fistula, was observed in 28.8% of patients (19 out of 66), while 21.2% developed new complications, including meatal stenosis, fistula, complete or partial breakdown, and urethral stricture. After the first salvage procedure, 27.7% of patients required further surgeries, with the majority (13 patients; 72%) needed just 1 procedure, 3 (16%) needed 2 procedures, 1 (5%) patient needed 3 procedures, and an additional 1 (5%) needed 4 procedures. The relatively lower complication rate observed after reoperation compared to primary surgery may be attributed to the predominant cause of reoperation in our setting—urethrocutaneous fistula (UCF). UCF generally has a high success rate after surgical correction, unlike strictures or breakdowns, which are more complex to manage. Similar findings were reported by Li et al in China, where fistula recurrence was the most frequent complication post-reoperation, with higher cure rates for fistulas, but lower outcomes for strictures after subsequent repairs.7,20 This underscores the escalating complexity of achieving satisfactory outcomes with successive procedures, highlighting the critical importance of minimizing failure rates in initial repairs to reduce the necessity for challenging reoperations.
The financial burden of re-operative hypospadias surgery extends beyond direct medical costs, affecting family income and stability. In Kenya, where the average annual household income is approximately KES 240,000 ($2300 USD), surgery costs ranging from KES 100,000–300,000 ($880–$2600 USD) represent a substantial portion of family earnings, particularly when multiple procedures are required. Indirect costs, including travel, accommodation, and lost wages due to hospital stays, further strain households, often necessitating that one parent, typically the mother, remain with the hospitalized child. Extended hospitalizations averages about 16 days, disrupting schooling, socialization, and play, which are critical for children’s development, emotional expression, and stress management. Repeated surgeries on sensitive areas can also affect psychological well-being, potentially lowering self-esteem and increasing anxiety related to body image. The complexity of re-operative cases, combined with the absence of standardized management guidelines, underscores the need for uniform protocols to improve surgical outcomes and address both functional and psychosocial impacts. Collaborative efforts within the surgical community could help refine techniques and enhance consistency in care.21,22
To reduce hypospadias complications and avoid reoperations, improvements in surgeon and nursing training, operational protocols, and capacity-building are essential, particularly in resource-limited settings like Kenya. Studies recommend specialized training focused on surgical techniques for hypospadias repair, meticulous attention to post-operative care, and dedicated educational programs for both surgeons and nurses. This includes practical training on complex repairs, use of specialized fine instruments, and effective handling of surgical complications, which are crucial to minimizing the risk of adverse outcomes and ensuring the best surgical results.23
Resource constraints, however, often impede the ideal post-operative protocol, particularly regarding equipment. Limited access to specific catheters, sutures, and sterile operating environments can increase complication rates. To address these challenges, some initiatives, such as partnerships between local and international surgical bodies, focus on equipping local facilities with necessary tools and fostering skills transfer through structured workshops and mentorship programs. These partnerships also emphasize protocol standardization and the importance of continuous monitoring of surgical outcomes, which can help identify and improve upon high-risk procedures. In cases where reoperation is necessary, protocols suggest a multidisciplinary approach involving both skilled surgeons and trained support staff. It is recommended to have specific guidelines for preoperative planning and patient care, alongside procedures to handle limited resources. This structured approach can help streamline the patient journey, from initial assessment to post-operative care, ultimately reducing the burden on both the health care system and the families involved.24
Recent advances in hypospadias repair are focused on improving outcomes and minimizing the need for reoperation. One significant area of progress is tissue engineering, which aims to use cell-seeded scaffolds or acellular matrices to regenerate urethral tissue. For example, studies on using buccal mucosa and acellular bladder matrices show promise in complex urethral reconstructions, especially in cases where the tissue lacks elasticity or is inadequate for standard repairs. Additionally, some research is exploring synthetic scaffolds and 3D bioprinting to produce urethral tissue that better integrates with the body’s natural tissues, potentially reducing post-surgical complications and improving functional outcomes.25
Another innovative approach in hypospadias treatment includes bioactive materials combined with regenerative medicine techniques, such as small intestinal submucosa and extracellular matrix materials, which help with cellular ingrowth and encourage more natural tissue development. Advances in 3D bioprinting are also opening avenues for creating anatomically precise scaffolds, enhancing the accuracy and success rates of these surgeries.26 On the preventive side, studies into the genetic and environmental factors associated with hypospadias are ongoing. Environmental exposures, particularly to endocrine-disrupting chemicals during pregnancy, have been linked to increased hypospadias risk. Greater awareness and prevention of these exposures may help reduce incidence rates in the long term.26
Limitations
This study is retrospective in nature and, as such, faced typical limitations related to data integrity, such as the possibility of unrecorded data. These limitations could have influenced the study’s findings. To mitigate this, both electronic and manual retrieval of patient medical records were conducted using identification numbers to ensure comprehensive data collection.
To address the issue of incomplete records, an independent data verification protocol was implemented. This involved separate data retrieval and cross-verification by principal investigators and research assistants, enhancing the reliability of the dataset used in the analysis.
Conclusions
In this retrospective review of hypospadias cases over a decade, the authors demonstrate that re-operative surgery significantly impacts patient outcomes, with some cases requiring up to 5 procedures to achieve a straight urinary stream and penile alignment. Salvage surgeries carry a risk of recurring complications, most commonly urethrocutaneous fistula, and present a likelihood of new complications, notably meatal stenosis, following failed primary repairs. Interestingly, the rate of failure in primary repairs was found to be comparable between distal and proximal hypospadias cases. Reoperations also extend the mean length of hospital stays and contribute to substantial social and economic burdens, emphasizing the critical need for successful primary repairs to minimize the need for complex, repeated procedures.
Acknowledgments
I am profoundly grateful to my wife and son, whose unwavering love and support have been my greatest source of strength throughout this journey. To my parents and siblings, my biggest fans, your constant encouragement and belief in me have been invaluable.
I extend my heartfelt appreciation to my supervisors, who walked with me every step of the way, guiding and mentoring me with wisdom and patience.
A special thank you to the Foreign Missions Board of the Southern Baptist Convention and Sharing Hope International for their generous support and steadfast belief in my vision. Your contributions have made this journey possible, and for that, I am deeply thankful.
Ethical Approval
This study was approved by the institutions’ ethics and research committee (KNH/UON-ERC, REF No. P503/052023).
Informed Consent
This study involved a retrospective review of patient records. As no direct patient contact occurred and all data were anonymized prior to analysis, informed consent was not required. Institutional ethical approval covered the use of retrospective data.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request. All patient information has been de-identified to protect confidentiality.
Conflict of Interest
The authors declare that they have no conflicts of interest related to this study.
Funding
This research did not receive any specific funding from public, commercial, or not-for-profit agencies.